Today’s Morning Report was originally presented by Dr. Tan on 5/7/2012:
Left Ventricular Assist Device (LVAD)
- Indications:
- New York Heart Association class 4 heart failure
- Ejection fraction <25%
- VO2 max less than 15 among other criteria
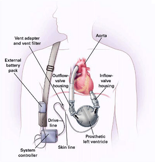
- How does it work:
- Bypasses left ventricle function.
- External pump unit outside body with intake channel (blood is drained from the apex of the left ventricle) and output channel (blood is ejected into the aorta).
- Note: BiVAD bypasses both ventricles.
- When would they come to the ED?
- Infections
- Driveline infections
- Overwhelming sepsis is unlikely but these infections can be difficult to treat once the patient is colonized
- Infections
- Bleeding – major problem with LVADs
- Anti-coagulation typically recommended for the majority of patients with LVAD
- Even if not, can develop acquired Von Willebrand disease (similar to patients on dialysis or with aortic stenosis) and angiodysplasias
- If the patient stops their Coumadin, are they going to have a thromboembolic event? UNLIKELY
- The patient is in extremis, altered or not breathing. You check and there is no pulse. Is the patient coding?
- Listen to the heart to make sure the pump is working (“like a muffled blender”).
- If the pump is not working, the patient is coding! You need to get the pump working…FAST
- Check all the wiring; controller, batteries, cables.
- Check for power!
- If it is working, there are several things you need to do.
- You need to get a MAP using Doppler.
- You need to get a monitor/EKG to look for evidence of RV problems (eg arrhythmias, STEMI)
- Cardiac echo via bedside ultrasound
- Things that can go wrong
- Pulmonary hypertension
- Decreases amount of blood that reaches the LVAD
- Exacerbated by acidosis and hypoxia. Consider intubation and bicarb
- Echo helpful – if you see a large right ventricle and a small left ventricle, think about pulmonary hypertension
- Thrombosis of the pump – consider heparin
- Consider inotropes in these patients
- Right heart failure –> consider milrinone or dobutamine
- Sepsis –> levophed
- Also think about PE
- Pulmonary hypertension
Thanks Dr. Tan, please leave any comments below!
The views expressed on this blog are the author's own and do not reflect the views of their employer. Please read our full disclaimer here. Any references to clinical cases refer to patients treated at a virtual hospital, Janus General Hospital.
The following two tabs change content below.


Jay Khadpe MD
Editor in Chief of "The Original Kings of County"
Assistant Professor of Emergency Medicine
Assistant Residency Director
SUNY Downstate / Kings County Hospital
Latest posts by Jay Khadpe MD (see all)
- Morning Report: 7/30/2015 - July 30, 2015
- Morning Report: 7/28/2015 - July 28, 2015
- IN THE STRETCHER INSTEAD OF BESIDE IT - July 22, 2015
- Morning Report: 7/14/2015 - July 14, 2015
- Morning Report: 7/10/2015 - July 10, 2015


