Here’s Dr. Caputo with an overview of the presentation, diagnosis, and management of Fournier’s Gangrene:
FOURNIER’S GANGRENE
Rapidly progressing necrotizing fasciitis involving the perineal, perianal, or genital regions and constitutes a true surgical emergency with a potentially high mortality rate (15-50%)
The rate of fascial necrosis has been noted to be as high as 2–3 cm per hour. NEED EARLY DIAGNOSIS AND TREATMENT
Fournier gangrene is most commonly found in middle-aged men (mean age, 50–60 years). 10 x more likely in males
MOST OFTEN due to a local infection adjacent to a point of entry, including abscesses (particularly in the perianal, perirectal, and ischiorectal regions), anal fissures, and colonic perforations.
Urologic sources: urethral strictures, chronic urinary tract infection, neurogenic bladder, recent instrumentation, and epididymitis
COMMON PREDISPOSING CO-MORBIDITIES: DM, Morbid obesity, Cirrhosis, Vascular disease of the pelvis, Malignancies, High-risk behaviors (eg, alcoholism, intravenous drug abuse), Immune suppression
MOST COMMON CAUSATIVE ORGANISMS: Usually polymicrobial: Streptococcal species, Staphylococcal species, Enterobacteriaceae family, Anaerobic organisms, Fungi
Presentation
The hallmark of Fournier gangrene is intense pain and tenderness in the genitalia. The clinical course usually progresses through the following phases:
- PRODROMAL SYMPTOMS: fever and lethargy, for ~ 2-7 days
- Intense genital pain and tenderness that is usually associated with edema of the overlying skin
- Dusky appearance of the overlying skin; subcutaneous crepitation. CREPITUS IN 19-64%
- Obvious gangrene of a portion of the genitalia; purulent drainage from wounds
- VARIABLE SYSTEMIC EFFECTS
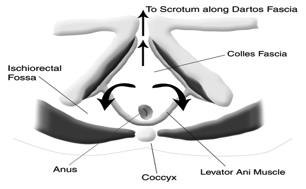
Relevant Anatomy
FASCIAL PLANES:
COLLES FASCIA: superficial perineum, if interrupted: buttocks/thighs
DARTOS FACIA: scrotum and penis
BUCK’S FASCIA: penis
SCARPA’S FASCIA: anterior abdominal wall
WORK UP
Laboratory Studies: SHOTGUN: PRE-OP LABS, BLOOD CULTURES
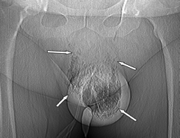
Imaging: Although the diagnosis of Fournier gangrene is often made clinically, imaging important
-Plain films: may reveal moderate-to-large amounts of soft-tissue gas or foreign bodies. Rapid but not the best test
Ultrasonography: can be used, BUT can it be tolerated. Important if torsion or epididymitis suspected
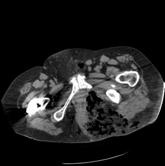
CT scanning: should be considered the diagnostic tool of choice. Can lead to early diagnosis with accurate assessment of disease extent. CT not only helps evaluate the perineal structures that can become involved by Fournier gangrene, but also helps assess the retroperitoneum, to which the disease can spread
MRI: greatest yield but not practical, do NOT want to delay
TREATMENT: INTENSE MEDICAL THERAPY AND EARLY SURGERY
Medical Therapy
Systemic toxicity: AGGRESSIVE resuscitation
EARLY Broad-spectrum antibiotic therapy: Need to cover staphylococci, streptococci, the Enterobacteriaceae family of organisms, and anaerobes.
If streptococci are the identified major pathogens, the drug of choice (DOC) is penicillin G, with clindamycin as the alternative. To ensure adequate treatment, there must be coverage for aerobic and anaerobic bacteria. The anaerobic coverage can be provided by metronidazole or third-generation cephalosporins. Gentamicin, combined with clindamycin or chloramphenicol, has been proposed as a standard coverage. Ampicillin may be added to the basic regimen to treat enterococci if suspected by Gram stain. MRSA à VANCO
Antifungals post op if tissue stains (ie, KOH stain) show fungi
Possibly HBO
Surgical Therapy
The definitive diagnosis of Fournier gangrene is established by examination in the OR: If frankly gangrenous tissue is found or purulence is drained
All necrotic tissue must be excised. The skin should be opened widely to expose the full extent of the underlying fascial and subcutaneous tissue necrosis. All fascial planes that separate easily with blunt dissection should be considered involved and therefore excised.
Possible fecal or urinary diversion, case specific
Orchiectomy if testicle is necrotic
AFTER THE EMERGENCY DEPARTMENT:
Antibiotics continued for 10-14 days or until reconstruction is accomplished.
Vacuum-assisted closure (VAC) for wound healing
Reconstruction/Graft
Complications: Unresolved sepsis, extension, complications
Outcome and Prognosis: Fournier Gangrene Severity Index (FGSI) based on deviation from reference ranges of 9 clinical parameters (temperature, heart rate, respiratory rate, white blood cell count, and levels of sodium, potassium, creatinine, hematocrit, sodium bicarbonate). Each parameter was valued between 0 and 4, with the higher value assigned to the greatest deviation from normal. The FGSI represents the sum of all the parameters values. They determined that advanced age (not a factor in the FGSI) and a FGSI greater than 9 correlated with increased mortality.
Thanks Dr. Caputo for today’s Morning Report! Leave any comments below.
Jay Khadpe MD
Latest posts by Jay Khadpe MD (see all)
- Morning Report: 7/30/2015 - July 30, 2015
- Morning Report: 7/28/2015 - July 28, 2015
- IN THE STRETCHER INSTEAD OF BESIDE IT - July 22, 2015
- Morning Report: 7/14/2015 - July 14, 2015
- Morning Report: 7/10/2015 - July 10, 2015


2 comments for “Morning Report: 5/21/2012”