Thank you to Dr. Melendez for today’s Morning Report!
Tylenol Overdose
Pathophysiology
- Acetaminophen (APAP) is rapidly absorbed from the stomach and small intestine and primarily metabolized by conjugation in the liver to nontoxic, water-soluble compounds that are eliminated in the urine.
- In acute overdose or when the maximum daily dose is exceeded over a prolonged period, metabolism by conjugation becomes saturated, and excess acetaminophen (APAP) is oxidatively metabolized by the CYP enzymes to the reactive metabolite NAPQI.
- N -acetyl-p-benzoquinone imine (NAPQI) has an extremely short half-life and is rapidly conjugated with glutathione, a sulfhydryl donor, and is renally excreted. Under conditions of excessive NAPQI formation, or reduction in glutathione stores by approximately 70%, NAPQI covalently binds to the cysteinyl sulfhydryl groups of cellular proteins, forming NAPQI-protein adducts.
- An ensuing cascade of oxidative damage, mitochondrial dysfunction, and the subsequent inflammatory response propagate hepatocellular injury, death, and centrilobular (zone III) liver necrosis. Similar enzymatic reactions occur in extrahepatic organs, such as the kidney, and can contribute to some degree of extrahepatic organ dysfunction.
Maximum Daily Dose
- The maximum recommended daily dose of acetaminophen is 4 g in adults and 90 mg/kg in children.
- Toxicity is associated with a single acute acetaminophen (APAP) ingestion of 150 mg/kg or approximately 7-10 g in adults.
- The ingested amount at which toxicity may occur may be lower in the settings of chronic ethanol use, malnourishment, or diminished nutritional status, fasting, or viral illness with dehydration, or if substances or medications that are known to induce the activity of the CYP oxidative enzymes are being used.
Clinical Effects
- Because antidotal therapy is most effective when initiated within 8 hours postingestion, the clinician must obtain an accurate history of the time(s) of ingestion, the quantity, and formulation of APAP ingested, and any co-ingestants, which may delay APAP absorption
- Because a patient’s history may be inaccurate, the serum acetaminophen concentration is important for diagnosis and treatment, even in the absence of symptoms. After a single ingestion, N -acetylcysteine NAC therapy is guided by the serum APAP concentration.
Phase 1 (0-24 h)
Patients may be asymptomatic or report anorexia, nausea or vomiting, and malaise. Physical examination may reveal pallor and diaphoresis. A subclinical rise in serum transaminases levels begins at about 12 hours postingestion.
Phase 2 (18-72 h)
In this phase, patients generally have and exhibit right upper quadrant abdominal pain, anorexia, nausea, and vomiting. Tachycardia and hypotension may be present. There is a continued rise in serum transaminases levels. Toxicity is defined as serum AST or ALT levels greater than 1000 IU/L. Clinical evidence of end-organ (hepatic or occasionally renal) toxicity is often delayed 24-48 hours postingestion.
Phase 3 (72-96 h)
In addition to the presentation of nausea and vomiting in phase 2, patients also may exhibit centrilobular hepatic necrosis with continued abdominal pain and a tender hepatic edge, jaundice, coagulopathy (including gastrointestinal [GI] bleeding), hepatic encephalopathy, and renal failure. Death from multiorgan failure may occur in this stage.
Phase 4 (4 d to 3 wk)
In phase 4, patients may have complete resolution of symptoms and complete resolution of organ failure, or their condition may be fatal.
Antidote and Treatment
- N -acetylcysteine (NAC) is a precursor of glutathione and as such, increases glutathione conjugation of NAPQI.
- NAC also enhances sulfate conjugation of unmetabolized APAP, functions as an anti-inflammatory and antioxidant, and has positive inotropic effects.
- In addition, NAC increases local nitric oxide concentrations and promotes microcirculatory blood flow, enhancing local oxygen delivery to peripheral tissues.
- The microvascular effects of NAC therapy are associated with a decrease in morbidity and mortality even when NAC is administered in the setting of established hepatotoxicity.
- NAC is maximally hepatoprotective when administered within 8 hours of ingestion. When indicated, however, NAC should be administered regardless of the time since the overdose.
- Therapy with NAC has been shown to decrease mortality rates in late-presenting patients with fulminant hepatic failure, even in the absence of measurable serum APAP levels.
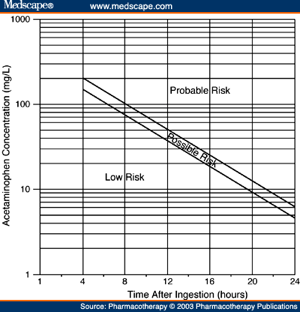
- A serum APAP concentration drawn 4 or more hours after a SINGLE ingestion may be plotted on the Rumack-Matthew nomogram as a guide to the likelihood of potential hepatotoxicity and the indication for NAC therapy.
- The nomogram is NOT applicable in the cases of multiple or chronic acetaminophen ingestion. In addition, it may be less reliable for the prediction of hepatotoxicity in cases of APAP ingestion that also includes anticholinergic agents or opioids, or in the case of extended-release APAP formulations.
Prognosis
- With aggressive supportive care in conjunction with antidotal therapy, the mortality rate for acetaminophen (APAP) hepatotoxicity is less than 2%.
- If correctly treated in a timely manner, most patients do not suffer significant sequelae; thus, patients who survive should be expected to have a return of normal hepatic function.
- Case series report that fewer than 4% of patients who suffer severe hepatotoxicity develop hepatic failure; fatalities or liver transplantation occurs in less than one half of these patients.
Rumack-Matthew Nomogram for NAC Administration
PO (72 hour course)
Loading dose is 140mg/kg PO, then 17 more doses every 4 hours of 70mg/kg PO. If patient vomits within 1 hour of receiving a dose, it must be repeated.
IV (21 hour course)
Patients >40 kg:
- Loading Dose: 150 mg/kg in 200 mL of diluent administered over 60 min
- Dose 2: 50 mg/kg in 500 mL of diluent administered over 4 hr
- Dose 3: 100 mg/kg in 1000 mL of diluent administered over 16 hr
Patients >20 – <40 kg:
- Loading Dose: 150 mg/kg in 100 mL of diluent administered over 60 min
- Dose 2: 50 mg/kg in 250 mL of diluent administered over 4 hr
- Dose 3: 100 mg/kg in 500 mL of diluent administered over 16 hr
Patients <20 kg:
- Loading Dose: 150 mg/kg in 3 mL/kg of body weight of diluent administered over 60 min
- Dose 2: 50 mg/kg in 7 mL/kg of body weight of diluent administered over 4 hr
- Dose 3: 100 mg/kg in 14 mL/kg of body weight of diluent administered over 16 hr
Leave any comments below.
Jay Khadpe MD
Latest posts by Jay Khadpe MD (see all)
- Morning Report: 7/30/2015 - July 30, 2015
- Morning Report: 7/28/2015 - July 28, 2015
- IN THE STRETCHER INSTEAD OF BESIDE IT - July 22, 2015
- Morning Report: 7/14/2015 - July 14, 2015
- Morning Report: 7/10/2015 - July 10, 2015