For today’s Morning Report, we have a review of Leptospirosis by Dr. Caputo:
Leptospirosis Morning Report
When should we consider it?
–>Leptospirosis should be considered when a patient has a flulike disease with aseptic meningitis or disproportionately severe myalgia. Travel history important. Multi-organ involvement.
Leptospirosis is a disease that is caused by pathogenic spirochetes of the genus Leptospira. It is considered the most common zoonosis in the world. Most common in the tropics.
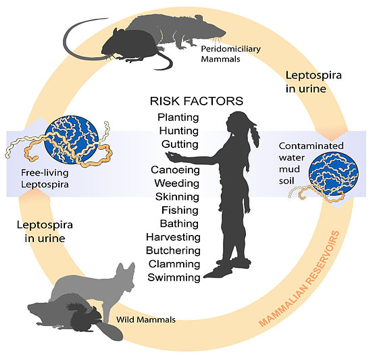
Urinary shedding of organisms from infected animals is the most important source of these bacterial pathogens. Contact with the organism via infected urine or urine-contaminated media results in human infection. Such media include animal bedding, soil, mud, and aborted tissue.
The organism enters the body via abraded skin or mucous membranes, such as the conjunctiva or alimentary tract. After the organism gains entry via intact skin or mucosa, it multiplies in blood and tissue. The resulting leptospiremia can spread to any part of the body but particularly affects the liver and kidney.
Despite the possibility of severe complications, the disease is most often self-limited and nonfatal.
Approximately 90% of patients manifest a mild anicteric form of the disease, and approximately 5-10% have the severe form with jaundice, otherwise known as Weil disease.
The natural course of leptospirosis falls into 2 distinct phases: septicemic and immune. During a brief period of 1-3 days between the 2 phases, the patient shows some improvement.
First stage: Septicemic/Leptospiremic stage
*Organism may be isolated from blood cultures, cerebrospinal fluid (CSF), and most tissues.
Duration: 4-7 days, the patient develops a nonspecific flulike illness: fever, chills, weakness, headache, chest pain, sore throat and myalgias, primarily affecting the calves, back, and abdomen.
Second stage: Immune/Leptospiruric
Circulating antibodies may be detected or the organism may be isolated from urine; it may not be recoverable from blood or CSF.
Duration: 0-30 days or more. Death is extremely rare in the anicteric cases.
Specific organ disease: include the meninges, liver, eyes, and kidney.
Neuro: Meningeal symptoms develop in 50% of patients. Aseptic meningitis is the most important clinical syndrome observed in the immune anicteric stage.
GI: Abdominal pain with diarrhea or constipation (30%), hepatosplenomegaly, nausea, vomiting, and anorexia can be seen. + Jaundice, elevated LFT’s
Renal: Azotemia, pyuria, hematuria, proteinuria, and oliguria are seen in 50% of patients with leptospirosis. ATN may occur during second week due to hypovolemia and decreased renal perfusion
Optho: Uveitis (2-10%) can develop early or late in the disease and has been reported to occur as late as one year after initial illness. Iridocyclitis and chorioretinitis are other late complications that may persist for years.
Pulmonary: Usually benign BUT is also main cause of death (Pulmonary hemorrhage, ARDS)
Skin/Musculoskeletal: Adenopathy, rashes (macular/maculopapular), and muscular pain are also seen.
Cardiac: Can have cardiovascular collapse: congestive heart failure, myocarditis, and pericarditis
Weil syndrome: is the severe form of leptospirosis and primarily manifests as profound jaundice, renal dysfunction, hepatic necrosis, pulmonary dysfunction, and hemorrhagic diathesis. 5-10 % mortality
Physical
- First stage: Common physical findings include fever; subconjunctival suffusion; pharyngeal injection; splenomegaly; hepatomegaly; mild jaundice; muscle tenderness; lymphadenopathy; and a macular, maculopapular, erythematous, urticarial, or hemorrhagic rash.
- Second stage: Physical findings depend on organ involvement.
- General – Adenopathy, rash, fever, bleeding, signs of hypovolemia/cardiogenic shock
- Icteric – Jaundice, hepatomegaly, abdominal tenderness, signs of coagulopathy
- Pulmonary – Cough, hemoptysis, dyspnea, respiratory distress
- Neurologic – Cranial nerve palsies, confusion, changes in consciousness, delirium, other signs of meningitis
- Ocular – Subconjunctival hemorrhage, uveitis, signs of iridocyclitis or chorioretinitis
- Hematologic – Bleeding, petechiae, purpura, ecchymosis, splenomegaly, abdominal tenderness
- Cardiac – Signs of congestive heart failure, pericarditis
Diagnosis
Definitive diagnosis is suggested by isolation of the organism by culture or a positive result on the microscopic agglutination test (MAT). MAT will not be positive until second week of illness
Cultures: Definitive diagnosis: Blood, urine, CSF. May miss in blood or CSF if it is too late
- Macroscopic slide agglutination test
- This test allows a presumptive diagnosis.
- Clinical illness consistent with leptospirosis must be present to support the diagnosis.
Blood work: Leukocytosis, elevated LFT’s, elevated bilirubin, elevated CPK, Azotemia, renal failure
Treatment:
NO human vaccine against leptospirosis is available.
Mild leptospirosis is treated with doxycycline, ampicillin, or amoxicillin.
For severe leptospirosis, the primary therapy is penicillin G, which is used widely in clinical practice. Cephalosporins also of value.
Thanks Dr. Caputo! Leave any thoughts below.
Jay Khadpe MD
Latest posts by Jay Khadpe MD (see all)
- Morning Report: 7/30/2015 - July 30, 2015
- Morning Report: 7/28/2015 - July 28, 2015
- IN THE STRETCHER INSTEAD OF BESIDE IT - July 22, 2015
- Morning Report: 7/14/2015 - July 14, 2015
- Morning Report: 7/10/2015 - July 10, 2015