Today we have a morning report from Dr. Auerbach with a review of intraosseous access!
IO:
Can I administer fluid rapidly? (up to 42ml/minute!)
IO vs IV?
Same time for medications to reach central circulation
Same delivery rate of fluid as central or peripheral IV when pressurized (which is preferred delivery method during resuscitation)
Indications:
Primary indication is cardiac arrest in infants
When cannot quickly establish access and need access
Contraindications:
Relative:
Osteoporosis and osteogenesis imperfect
Needle insertion through cellulitis, infection, or burns
Absolute:
Fractured bone
Recent IO placement in same bone
IO needles
-have EZ-IO
-Cook IO needle
Site:
Infants and children <6 years of age
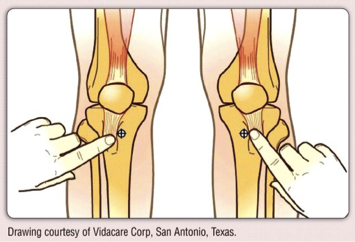
 Preferred site is proximal tibia (2 fingerwidths, (1-3cm) below the tuberosity, using the broad flat anteromedial side); this is to miss the growth plate
Preferred site is proximal tibia (2 fingerwidths, (1-3cm) below the tuberosity, using the broad flat anteromedial side); this is to miss the growth plate
Other viable sites are distal tiba, and distal femur (insertion site 2-3cm above the external femoral condyle in the midline, directed cephalad at a 10-15 degree angle)
Clavicle and humerus has been used but should be last resort
In older children and adults
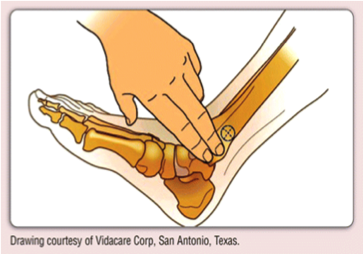
 Preferred site is distal tibia, site of needle insertion should be medial surface at the junction of the medial malleolus and tibia shaft, posterior to the saphenous vein; insert needle cephalad
Preferred site is distal tibia, site of needle insertion should be medial surface at the junction of the medial malleolus and tibia shaft, posterior to the saphenous vein; insert needle cephalad
Sternum can be used as a site in adults, can be more helpful in patients with extremity injuries or amputees
Actual procedure:
Place support behind knee (i.e. towel roll)
Clean well area of insertion
Anesthesia for conscious patients, otherwise not necessary
Stabilize the extremity with free hand (however keep out of insertion plane as to avoid puncturing your hand)
Direct IO needle either perpendicular or slightly caudal
Use twisting or rotating motion until feels a decrease in resistance (penetration usually is 1CM deep into bone)
Stabilize needle
Aspiration of blood or marrow confirms correct placement
Check for extravasation of fluid outside of bone (improperly placed IO)
Obviously for EZ-IO do not need all of above
What can I send?
HGBN, Glucose, pH, PCO2, HC03, Na, Cl, BUN, creatinine, Cultures, serum drug levels. Possibly can check type and Rh too.
Complications:
Hold needle with index finger 1 CM from bevel to prevent through and through insertion
If no free flow of fluid back, either:
1) Needle not through cortex, reinsert stylet and re-advance
2) Needle through and through, pull back on it and aspirate
3) Clogged by spicule or clot: flush with saline
4) If still not working, remove and choose another site
If have extravasation, must remove needle and apply pressure and retry elsewhere
Rarer complications include infection, compartment syndrome, epiphyseal injury, fat embolism and myonecrosis
Remember: check compartments for tissue extravasation
Also, cannot leave in for more than 24 hours
Source: Roberts and Hedges, 5th edition
Thanks Dr. Auerback! Leave any comments below.
Jay Khadpe MD
Latest posts by Jay Khadpe MD (see all)
- Morning Report: 7/30/2015 - July 30, 2015
- Morning Report: 7/28/2015 - July 28, 2015
- IN THE STRETCHER INSTEAD OF BESIDE IT - July 22, 2015
- Morning Report: 7/14/2015 - July 14, 2015
- Morning Report: 7/10/2015 - July 10, 2015
