Thank you to Dr. Meister for today’s Morning Report.
Postpartum Headache:
In a retrospective review of 95 women with severe postpartum headache, 39% were diagnosed with tension headache, 24% with preeclampsia/eclampsia, 16% with postdural puncture headache, 11% with migraine, and the remaining 10% with serious conditions such as intracranial hemorrhage, a mass, or cerebral venous sinus thrombosis. When the headache is accompanied by hypertension and proteinuria, the working diagnosis should be preeclampsia until proved otherwise. BUT High BP if in pain!
Pre-eclampsia:
Definition:
Systolic>140 OR diastolic >90 AND proteinuria ³ 0.3 g in 24 hour period (random >30mg/dL or >1+ on dipstick is suggestive but not diagnostic. CAN HAVE NO PROTEIN IN SPOT U/A!
Severe: SBP of 160 mm Hg or higher or DBP of 110 mm Hg or higher on 2 occasions, 5 grams protein/day/oliguria/cerebral or visual disturbances.
Epidemiology:
The incidence of preeclampsia in the United States is estimated to range from 2% to 6% in healthy, nulliparous women. Among all cases of the preeclampsia, 10% occur in pregnancies of less than 34 weeks gestation. The global incidence of preeclampsia has been estimated at 5-14% of all pregnancies.
Blood pressure rises progressively over postpartum days 1 through 5 and peaks on days 3 to 6 after delivery.
LPPE now represents about 13% to 16% of all cases of eclampsia. 48 hours to within 4 weeks of delivery. Case reports exist of 6-8 weeks postpartum.
The relative incidence of LPPE is rising. LPPE now represents about 13% to 16% of all cases of eclampsia.Reasons for this change in epidemiology may include early discharge after delivery and hence failure to detect the postpartum rise in blood pressure that peaks 5 to 6 days after delivery.
Factors that can be measured early in pregnancy that increase the likelihood of pre-eclampsia in any given pregnancy:
First pregnancy
Multiparous
Pre-eclampsia in any previous pregnancy
≥10 years since last baby
Age ≥40 years
Body mass index of ≥35
Family history of pre-eclampsia (mother or sister)
Diastolic blood pressure of ≥80 mm Hg at booking
Proteinuria (of ≥1+ on more than one occasion or quantified at ≥0.3 g/24 h) at booking
Multiple pregnancy
Certain underlying medical conditions*
*Pre-existing hypertension; pre-existing renal disease; pre-existing diabetes; antiphospholipid antibodies present.
Pathophysiology:
Many theories have been proposed about the pathophysiology of preeclampsia/eclampsia, including immunologic mechanisms, an enhanced systemic inflammatory state, a relative increase in oxidant activity, increased placental debris in the maternal circulation, the presence of circulating antibodies against angiotensin II receptors, and a prothrombotic state. Whatever the mechanism(s), the placenta is known to play a critical role in the pathophysiology of preeclampsia. Spiral arteries that remain narrow instead of developing into large, tortuous vascular channels can cause placental hypoperfusion. Vascular, environmental, immunologic, and genetic factors also appear to be involved. The ischemic placenta is believed to release factors into the maternal bloodstream that alter maternal endothelial cell function. All the clinical features of preeclampsia can be explained as responses to generalized endothelial dysfunction.
In eclampsia, the degree of brain edema correlates more strongly with markers of endothelial cell dysfunction than it does with the degree of hypertension,supporting the theory that endothelial cells play a role in this disorder. In a case series of 28 pregnant women with eclampsia and stroke, 15 of whom died, the mean systolic blood pressure was 175 mm Hg and the mean diastolic blood pressure was 98 mm Hg. Diastolic blood pressure was above 110 mm Hg in only 3 women and was above 105 mm Hg in only 5, suggesting that their strokes were not directly related to the absolute elevations in blood pressure
Complications:
Posterior reversible encephalopathy syndrome is a clinical and radiologic syndrome that includes headache, confusion, visual changes, and seizures and is accompanied by diagnostic white matter abnormalities seen on MRI. It is a rare—but potentially lethal—complication of eclampsia.
RENAL FAILURE
DIC
DEATH
BRAIN DAMAGE
ICH
ISCHEMIA
PULMONARY EDEMA
CVA
The most common cause of maternal death was cerebral hemorrhage
Presentation:
- Headache
- Nausea / Vomiting
- Visual disturbance
- RUQ / Epigastric pain
- Malaise
Physical Exam:
Altered mental status
Focal neurologic deficits
Reduced visual acuity
Hyperreflexia
Right upper quadrant or diffuse abdominal tenderness
Peripheral edema
Purpuric rash
Labs: LFT’s, LDH, uric acid- why? An overproduction of uric acid occurs when there is excessive breakdown of cells, or a kidney problem with the inability of the kidneys to excrete uric acid.
TREATMENT:
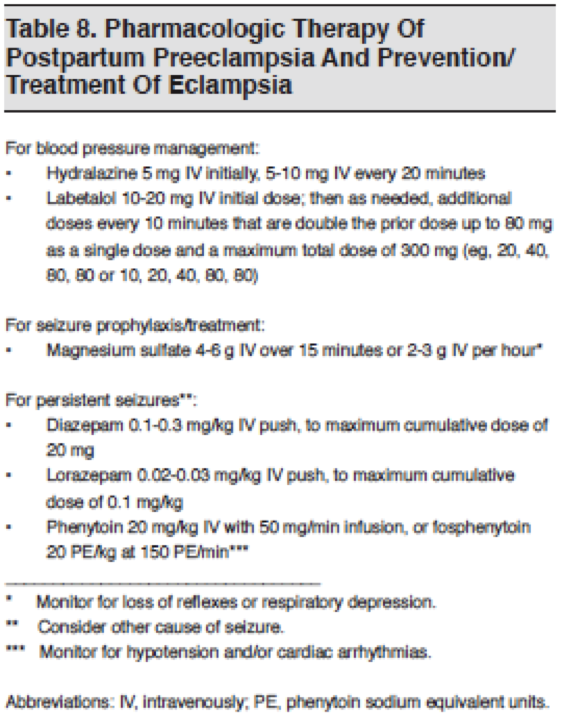
Although it is not clear whether elevated blood pressure is a cause or an effect of the pathophysiology of stroke in eclampsia, practice patterns and prudence suggest that—just as for the antepartum patient—the postpartum patient will benefit from careful, ongoing monitoring of blood pressure and lowering of blood pressures to 130 to 150 mm Hg systolic and 80 to 100 mm Hg diastolic.
Hydralazine/labetolol
Magnesium sulfate has been shown to be effective in this regard, reducing the risk of eclampsia by 50% compared with placebo. Seizures in eclampsia are usually of short duration and self-limited. In well-designed prospective studies, treatment with magnesium has also been shown to be more effective and safer in preventing further seizures in pregnant patients than either diazepam or phenytoin AND PREVENT MORTALITY. If it doesn’t work- treat it like status and consider other etiology.
Magnesium sulfate is given at a loading dose of 4 to 6 g IV over 15 minutes followed by 2 to 3 g IV per hour. Areflexia, particularly loss of the patellar deep tendon reflex, has been observed at 8 to 10 mEq/L, and respiratory paralysis seen at >13 mEq/L. Therapeutic goal is 4-7 mg/dL.
Watch out if renal failure, more prone to toxicity.
| Side effects: |
| ▪ hypotension secondary to reductions in systemic vascular resistance▪ facial flushing
▪ visual disturbances ▪ flushing at injection site ▪ chest pain ▪ nasal stuffiness ▪ dysrhythmia |
▪ circulatory collapse
▪ gastro-intestinal upset
▪ urinary retention
▪ magnesium toxicity
▪ tissue necrosis at injection site
The Pritchard regimen (which involves a slow intravenous [IV] injection of 4 g of magnesium sulfate [MgSO4] diluted in 20 mL of distilled water, with an intramuscular [IM] injection of 5 g of MgSO4 as the loading dose, followed by a 5-g IM injection of MgSO4 every 4 hours in alternate buttocks until 24 hours after the last convulsion or abortion/delivery—whichever occurs later) has been considered the gold-standard treatment.
More invasive approaches to severe LPPE:
In a case report of refractory seizures, 2 patients had rapid recovery after uterine curettage. In another case report, plasma exchange reportedly resulted in a full recovery. Cerebral angioplasty improved outcome in 1 patient with neurologic deficits in one reported case.
Atypical preeclampsia
| Gestational hypertension plus ≥ 1 of the following items: |
| Symptoms of preeclampsia |
| Hemolysis |
| Thrombocytopenia (< 100,000/mm3) |
| Elevated liver enzymes (2 times the upper limit of the normal value for aspartate aminotransferase or alanine aminotransferase) |
| Gestational proteinuria plus ≥ 1 of the following items: |
| Symptoms of preeclampsia |
| Hemolysis |
| Thrombocytopenia |
| Elevated liver enzymes |
| Early signs and symptoms of preeclampsia-eclampsia at < 20 weeks of gestation |
| Late postpartum preeclampsia-eclampsia (> 48 hours after delivery) |
Sibai. Diagnosis and management of a typical preeclampsia-eclampsia. Am J Obstet Gynecol 2009.
Diagnostic modality that is also considered is the measurement of uterine artery Doppler velocimetry that shows the classic “notching” characteristic of increased resistance in the placenta of patients with preeclampsia. The sensitivity of this test in patients with established early onset preeclampsia ranges from 87-96%.
Leave any thoughts below.
Jay Khadpe MD
Latest posts by Jay Khadpe MD (see all)
- Morning Report: 7/30/2015 - July 30, 2015
- Morning Report: 7/28/2015 - July 28, 2015
- IN THE STRETCHER INSTEAD OF BESIDE IT - July 22, 2015
- Morning Report: 7/14/2015 - July 14, 2015
- Morning Report: 7/10/2015 - July 10, 2015