E-FAST. What do the letters stand for?
Extended Focused Assessment with Sonography for Trauma (as opposed to FAST- Focused Assessment with Sonography for Trauma)
How is E-FAST different than the FAST?
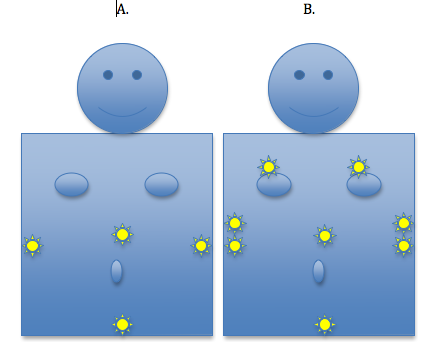
There are 4 anatomical spaces examined in the FAST: Hepatorenal space (Morison’s Pouch), Splenorenal space, Rectovesicular space (Pouch of Douglas in females) and Pericardial space
The E-FAST is “extended” in that it includes bilateral views of the hemithoraces.
Below is a crude image of anatomical points of examination of the FAST exam (A) and E-FAST exam (B). Please read next section for clarification of exact anatomical positions.
How do I examine the hemithoraces in the E-FAST?
Generally to check for a pneumothorax, look at the anterior apices of the lung and to check for a hemothorax, the dependent areas of the lower lung should be viewed. This is because, in a supine patient, hemothoraces settle posteriorly and pneumothoraces anteriorly.
Bilateral Anterior Hemithoraces
Take the probe and place it with indicator pointing cephalad in the 2nd-3rd intercostal space in the mid-clavicular line. Slide caudally to evaluate for a pneumothorax.
Bilateral Pleural Spaces
Checking these spaces should be incorporated into the FAST during the examination of the hepatorenal and splenorenal spaces.
The right pleural space will be viewed at the anterior axillary line at the 6th to 9th intercostal spaces. After viewing the hepatorenal space, slide the probe cephalad one rib space above the diaphragm. If there is a rib shadow, turn the indicator clockwise 30 degrees to get in between the rib space.
The left pleural space will be viewed at the posterior axillary line at the 4th to 8th intercostal spaces. After viewing the splenorenal space, slide the probe cephalad one rib space above the diaphragm. If there is a rib shadow, turn the indicator clockwise 30 degrees to get in between the rib space.
www.acep.org. Resa E. Lewiss. Focus on EFAST. January 2009.
What probe do I use?
You can use the curvilinear probe, same as for a FAST. You may consider switching to a linear probe for the anterior thoracic approach.
Why is the E-FAST better than the FAST?
Well, because it includes noninvasive, expedited detection of intrathoracic injury in an acute setting. It allows for the detection of pneumothorax with higher sensitivity than supine AP chest x-ray: 86-98% by ultrasound, as compared with 28-75% by CXR. (The specificity of both techniques is 100%).
Does evidence support use of the E-FAST?
Yes.
Here’s some evidence supporting ultrasound detection of pneumothorax in trauma patients:
Blaiyas M. Lyon M. Duggal S. A prospective comparison of supine chest radiography and bedside ultrasound for the diagnosis of traumatic pneumothorax. Acad Emerg Med. 2005 Sep: 12 (9): 844-9.
This study compared the sensitivity and specificity of bedside ultrasound in the ER with supine portable AP chest radiography in detecting pneumothoraces in trauma patients and to see if ultrasound could grade the size of the pneumothorax. It was a prospective, single-blinded study at a level 1 trauma center. Enrollment criteria: adult ER patients, pts to receive CT including lung windows. Attending ER physicians performed bedside trauma US, portable, supine AP chest radiographs were evaluated by attending trauma physician blinded to the results of the thoracic ultrasound. CT results or air release on chest tube placement were compared with Ultrasound and CXR findings. Total patients enrolled over a 8-month period: 176. Results showed a sensitivity of US to be 98% as compared with 75% for supine AP CXR. Specificities for both techniqes were at 100% The ultrasound method allowed for a differentiation between small, medium and large pneumothoraces with good agreement with CT results.
Soldati G et al. Occult traumatic pneumothorax: diagnostic accuracy of lung ultrasound in the emergency department. Chest. 2008 Jan:133 (1): 204-11
This study was an 18-month prospective study of 109 pts admitted to ED for chest trauma or polytrauma. Pts received a spiral CT chest and AP supine CXR within 1 hour of ED admission. Lung ultrasound was carried out by an operator blinded to examination results. 25 PTX detected. Ultrasound was found to have a sensitivity of 92%, specificity of 99.4%. AP supine CXR was found to have a sensitivity of 52% and specificity of 100%. Of 25 PTX, in 20 reads, there was agreement on extension of the PTX between CT and US, chest xray was unable to give quantitative results.
(Our very own!!!)
Wilkerson RG, Stone MB. Sensitivity of bedside ultrasound and supine anteroposterior chest radiographs for the identification of pneumothorax after blunt trauma. Acad Emerg Med. 2010 Jan; 17 (1): 11-7.
This study was an evidence-based review of trials from 1965 to 2009. Inclusion criteria: pneumothorax suspected, age >18, ER patients. Ultrasound was performed by ED physicians. Exclusion criteria: radiologist or surgeon performed ultrasound, penetrating trauma, iatrogenic or spontaneous pneumothoraces. 606 patients met criteria. CT or rush of air during tube thoracostomy was the standard for presence or absence of pneumothorax. The investigators found (as quoted in the previous question) the sensitivity/specificity of ultrasound in detecting pneumothorax: 86-98%/100%, respectively; the sensitivity/specificity of supine AP CXR in detected pneumothorax: 28-75%/100%, respectively.
Nandipati KC et al. Extended focused assessment with sonography for trauma (EFAST) in the diagnosis of pneumothorax: experience at a community based level 1 trauma center. Injury. 2011 May: 42 (5):511-4.
This was a prospective study over 12 months of 204 trauma patients, both blunt and penetrating trauma patients were assessed. EFAST performed by surgeons in the ED, clinical examination by surgeons, supine AP CXR was obtained and compared with CT scan findings. 21 patients were included, clinical examination picked up 17 PTX, supine AP radiograph picked up 16 PTX and ultrasound picked up 21 out of 21 PTX.
What about for hemothorax?
Well the evidence isn’t as overwhelming, more studies need to be done.
Ma OJ, Mateer JR. Trauma ultrasound examination versus chest radiography in the detection of hemothorax. Ann Emerg Med. 1997 Mar; 29 (3):312-6.
In this prospective, 17-month, analysis of 245 trauma patients at a level 1 center. AP supine CXR and ED physician bedside ultrasound were equal in detecting hemothorax at a sensitivity and specificity of 96% and 100%, respectively as compared with CT.
Abboud PA, Kendall J. Emergency department ultrasound for hemothorax after blunt traumatic injury. J Emerg Med. 2003 Aug; 25 (2):181-4
Prospective study over 11 month period. 142 trauma patients included in the study. 16 cases of hemothorax found by the gold-standard, CT chest. ED ultrasound was 12.5% sensitive and 98% specific in detecting hemothorax. The low sensitivity being in large part due to the inability of US to detect small-volume hemothorax detected by CT.
What are the limitations of E-FAST, specifically the thoracic portion of the ultrasound?
False-positives in patients with apnea, mainstem bronchus intubation, adherent lung.
Ultrasound does not replace CXR. Initial CXR is still important in trauma patients to detect lung parenchymal and mediastinal injury.
What are the take-home points here?
Learning E-FAST is useful. It leads to a quick diagnosis of intrathoracic injury that can save your patient’s life. It’s non-invasive and extremely useful in providing fast, bedside information in a trauma patient. Serial exams are easy to perform and give you a lot of information.
E-FAST is more sensitive than bedside CXR at detecting pneumothorax and may be as sensitive in detecting hemothorax in trauma patients.
sadia.hussain
Latest posts by sadia.hussain (see all)
- A Critical Care Frequent Flyer: Stroke - October 14, 2014
- As if Math Wasn’t Traumatic Enough… Calculating Injury Severity Scores - October 13, 2014
- Congeal your knowledge on Thromboelastography… Read on! - July 22, 2014
- I Saw the Pediatric Seatbelt Sign and It Opened Up My Eyes… I Saw the Sign. - June 9, 2014
- Trauma Patient, No IV…CT With IO Contrast? - April 13, 2014