Today’s Morning Report is courtesy of Dr. DiMare!
Sedation and the Agitated Patient
What are the hallmarks of delirium?
– altered level of consciousness
- either increased or decreased
– disturbances in sleep/wake cycle
– generally caused by illness, medication or intoxication
– caused by imbalance of neurotransmitters
- dopamine, seratonin, acetylcholine, GABA
What should our focus be?
– diagnosing the underlying cause may be the final solution
– safety of patient and staff while finding the underlying cause
– don’t make things worse
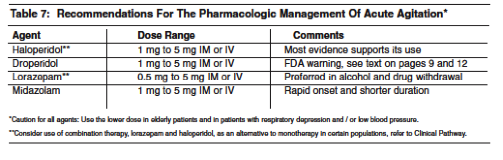
What do we generally use?
– High potency Typical Antipsychotics
- Haloperidol
- Droperidol
– Benzos
- Midazolam
- Lorazepam
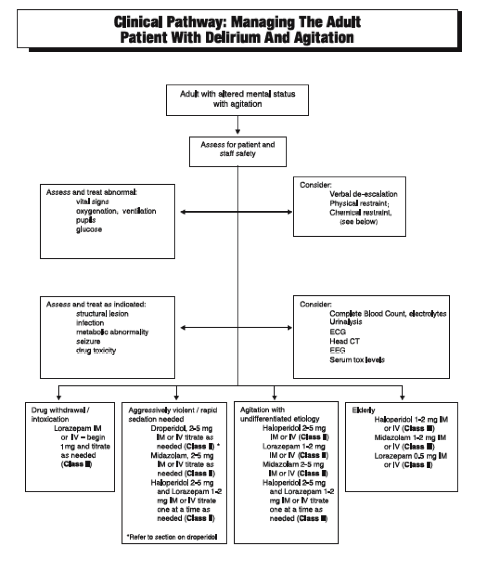
Who needs to be sedated? And how?
– Intoxicated and crazy
- Actively intoxicated
- ETOH – haldol/droperidol
- Droperidol is quicker acting than haldol
- Less chance of respiratory depression
- EKG once sedated since EtOH puts you at risk for hypomagesemia and long QTc
- Sympathimomimetics (cocaine/PCP) – Benzos
- Less of a concern for respiratory suppression
- ETOH – haldol/droperidol
- EtOH withdrawal – Benzos
- Treat withdrawal and you will treat the agitation
- Generally not Midazolam – may need to be re-dosed, documented instances of respiratory depression requiring BVM or intubation after multiple rounds of re-dosing
- Combo therapy
- Considered safe in the generally young, intoxicated population, allows shorter onset and longer duration and minimizes side effects of both drug classes
– Old and crazy
- Typical teaching has been that haldol is better than benzos
- Best treatment is to treat the cause but sedation is often necessary to allow full evaluation
- Haldol
- Cochrane Review – decreases aggression, doesn’t decrease agitation
- Droperidol – typically avoided because of “black box” warning
- Benzos
- May be better if patient has Parkinsons
- Less of a chance of EPS
- Avoid in a hypotensive patient or a patient who may be on their way to being hypotensive (ie delirium secondary to infection)
- May be better if patient has Parkinsons
- All of these patients should be admitted
– Just crazy
- Longer periods of agitation lead to more violent outbursts, often unprovoked
- American Psychiatrists Assoc recommends Haldol as first line medication
- Droperidol may be superior because of shorter time to onset, longer half life, increased potency
- Review of 12,000 patients who received droperidol for primary psychotic behavior showed no dysrhythmias
After sedating:
– VS including FSG
– put the patient on a monitor
– get an EKG
– try not to physically as well as chemically restrain
– examine the patient for signs of trauma
– if things don’t make sense do more tests
- CT head, LP, chemistry etc.
Thanks Dr. DiMare!
Jay Khadpe MD
Latest posts by Jay Khadpe MD (see all)
- Morning Report: 7/30/2015 - July 30, 2015
- Morning Report: 7/28/2015 - July 28, 2015
- IN THE STRETCHER INSTEAD OF BESIDE IT - July 22, 2015
- Morning Report: 7/14/2015 - July 14, 2015
- Morning Report: 7/10/2015 - July 10, 2015