So to recap… our case was that of a 44yo F presenting from St. Vincents with fever, AMS and abdominal pain. Further pertinent negatives ans positives that were obtained through your questions were the following:
- No hx of DVT, abnormal rhythm, IVDU, valvular HD, HIV, hemoglobinopathy. No known medical problems. No FH of lupus. No current medications.
- Exam showed no murmur, RUQ tenderness w/o rebound/guarding, no jaundice, negative guiac
- Labs were significant for Anemia, Bandemia, Renal failure with uremia, thrombocytopenia, transaminitis, an acute respiratory alkalosis with appropriate metabolic compensation, no schistocytes or malaria parasites and normal coags
Our proposed diagnoses included TTP, malaria, atrial fibrillation, septic emboli from endocarditis, hemoglobinopathy, malaria, TB, disseminated crypto, malignancy, ascending cholangitis, ruptured ectopic, vasculitis, ATLL w/ HTLV, systemic histoplasmosis, dengue, Lupus and leptospirosis.
So where do we go from here… well first I’d like to fill in the blanks and give you some of the information that wasn’t asked for… things that you would likely do if you saw this patient yourself in the ER.
The one thing that wasn’t mentioned but is obvious in the setting of FEVER+AMS is LP. In this case the LP was actually not done until the pt got to the MICU. It was unclear as to why this was delayed… but regardless the results were negative for infection (high glucose, normal protein, 1WBC).
TTP was another diagnosis that was mentioned… and it’s a life threatening diagnosis that needs to be ruled out in the ED. Our patient has the classic pentad of Fever, Anemia,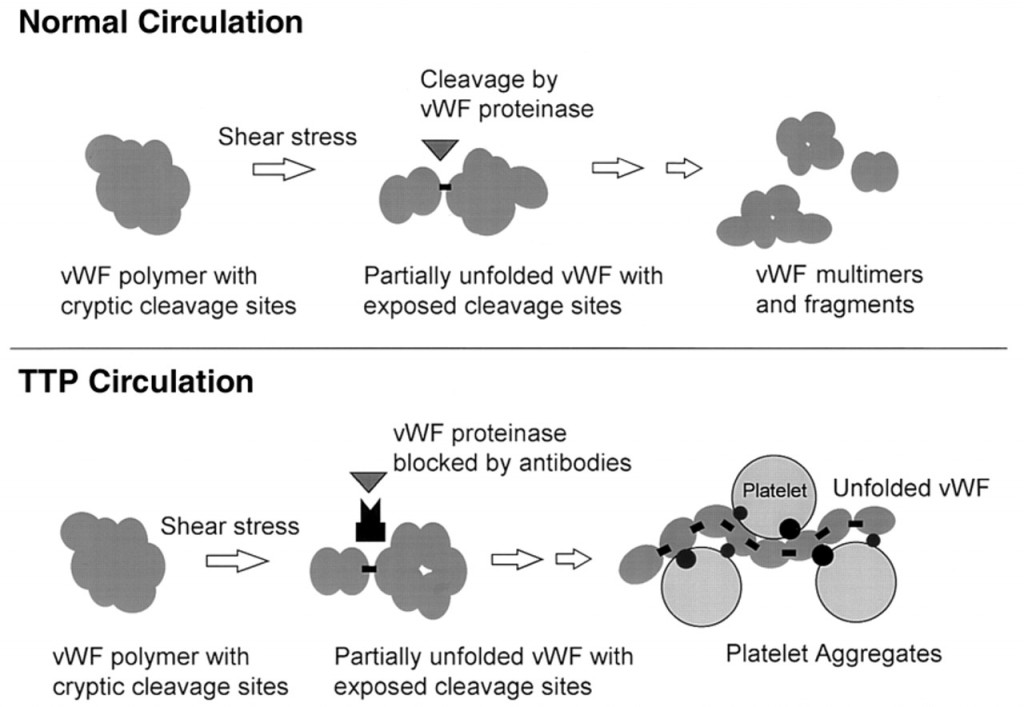 Thrombocytopenia, Renal failure and Neurologic manifestations. TTP is caused by a deficiency in a protein ADAMSTS13 which is responsible for cleaving multimers of von-Willebrand factor (vWF). vWF is responsible for crosslinking platelets and fibrin and helping to form clots. With excess vWF floating around, patients with TTP form clots in their microvasculature which consume platelets, shear RBCs and block blood supply to parts of the kidneys and brain. The only effective treatment for TTP is plasmapheresis which removes vWF multimers and provides normal ADAMSTS13. This treatment is often initiated in patients with suspected TTP even without all the clinical signs/symptoms since the morbidity and mortality of this disease is high (90%+ mortality if not treated).
Thrombocytopenia, Renal failure and Neurologic manifestations. TTP is caused by a deficiency in a protein ADAMSTS13 which is responsible for cleaving multimers of von-Willebrand factor (vWF). vWF is responsible for crosslinking platelets and fibrin and helping to form clots. With excess vWF floating around, patients with TTP form clots in their microvasculature which consume platelets, shear RBCs and block blood supply to parts of the kidneys and brain. The only effective treatment for TTP is plasmapheresis which removes vWF multimers and provides normal ADAMSTS13. This treatment is often initiated in patients with suspected TTP even without all the clinical signs/symptoms since the morbidity and mortality of this disease is high (90%+ mortality if not treated).
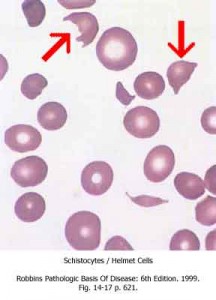 So… would you treat our patient? She demonstrates the classic pentad, but in order for this to really be TTP you must see schistocytes on the smear. The pathology of TTP comes from micro-clots in the circulation and while we cannot see those micro-clots, we can see their direct result -> shearing of RBCs which creates schistocytes. While schistocytes can be seen in other conditions as well as in normal patients studies suggest that they comprise less than 0.5% of all RBCs in normal patients while in TTP the number should be greater than 1%. However 1% schistocytes = 2 cells per high power field (100x) which sounds like a number that is easy to miss. Thus, if you are thinking TTP you need an experienced person interpreting the smear… which means HEMATOLOGY CONSULT even if schistocytes are not reported on the initial smear.
So… would you treat our patient? She demonstrates the classic pentad, but in order for this to really be TTP you must see schistocytes on the smear. The pathology of TTP comes from micro-clots in the circulation and while we cannot see those micro-clots, we can see their direct result -> shearing of RBCs which creates schistocytes. While schistocytes can be seen in other conditions as well as in normal patients studies suggest that they comprise less than 0.5% of all RBCs in normal patients while in TTP the number should be greater than 1%. However 1% schistocytes = 2 cells per high power field (100x) which sounds like a number that is easy to miss. Thus, if you are thinking TTP you need an experienced person interpreting the smear… which means HEMATOLOGY CONSULT even if schistocytes are not reported on the initial smear.
Long story short… hematology saw this patient… and the smear showed no schistocytes… but was not completely normal. Hematology commented on atypical lymphocytes AKA smudge cells… Going back to our CT, the official impression was hepatometagly, splenomegaly and lymphadenopathy. What can give these findings in the setting of anemia, thrombocytopenia and renal failure?
…
TUMOR LYSIS SYNDROME!!
Our patient’s final diagnosis was B-cell lymphoma and her initial presentation was that of tumor lysis syndrome secondary to increased cell turnover from her malignancy. Often we think of tumor lysis syndrome in the setting of a cancer patient undergoing chemotherapy and while that is a likely construct, it can also occur in the absence of chemotherapy. Typically in cases of liquid tumors, their high metabolic turnover can lead to release of intracellular ions and metabolic byproducts into the systemic circulation. The common laboratory findings include hyperuricemia, hyperkalemia, hyperphosphatemia, hypocalcemia and acute renal failure.
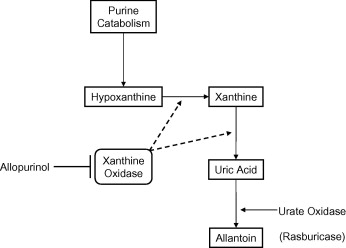
While electrolyte abnormalities like hyperkalemia and hypocalcemia can be immediately life-threatening, the morbidity from tumor lysis syndrome comes from renal failure which is mediated by hyperuricemia. Uric acid is created when the purines in DNA is metabolized by xanthine oxidase in the liver. While soluble in the plasma, uric acid become less soluble in urine due to its low pH. This leads to crystal formation which obstructs urine flow. In addition to uric acid crystals, the hyperphosphatemia from cell breakdown can cause precipitation of calcium phosphate crystals in the urine and further contribute to renal failure.
- FLUIDS, FLUIDS, FLUIDS. These patients may require upwards of 4-5 liters of fluid per day. The goal is for their urine output to be at least 3L. Aggressive fluid hydration helps correct electrolyte imbalances and increased blood flow to the kidneys. This increases the volume of urine produced which decreases the overall concentration of uric acid preventing crystal formation.
- Another treatment modality is to block the production of uric acid by blocking xanthine oxidase. Allopurinol is often used for prevention of hyperuricemia in patients undergoing chemotherapy.
- However, if patients are already hyperuricemic, allopurinol alone will not bring uric acid levels down. Rasburicase in synthetic urate oxidase which converts uric acid to allantoin to aid in excretion
- Alkalanization of the urine. Since uric acid is less soluble at low pH, bringing the pH up can prevent crystal formation. This is done through sodium bicarbonate infusion. Goal urine pH is 7.5 or a serum bicarbonate of 30mEq/L. However, alkalinization may decrease the solubility of calcium phosphate which leads to crystal formation. Thus, it is somewhat controversial.
Tumor lysis syndrome is a difficult diagnosis to make in the ED without the history of current chemotherapy. It is even more difficult if the patient does not have a diagnosis of malignancy. However, it is not impossible. There are certain tests that you can send and get results quickly which can raise your clinical suspicion, but like anything, unless you think about it, you won’t make the diagnosis. Sending a uric acid level and a LDH level can help you make this diagnosis… especially in the setting of renal failure, hepatomegaly and splenomegaly. In our patient, the uric acid level was over 11 and the LDH was over 2500.
nchristopher
Latest posts by nchristopher (see all)
- What’s wrong with this picture? – Answer - September 11, 2013
- What’s wrong with this picture? - August 21, 2013
- EKG Case 8 – Answer - July 16, 2013
- EKG Case 8 – All that wheezes - June 19, 2013
- EKG Case 7 Answer - June 19, 2013

1 comment for “X-ray Vision: Case 2 – Answer!”