Today’s Morning Report is courtesy of Dr. Caputo!
Penetrating Neck Injuries
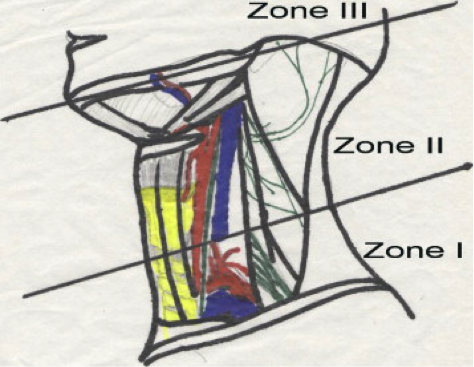
Zone I: Extends from the clavicle to the cricoid cartilage and includes the thoracic inlet Subclavian vessels, brachiocephalic veins, common carotid arteries, aortic arch, and jugular veins, trachea, esophagus, lung apices, cervical spine, spinal cord, and cervical nerve roots.
* Signs of a significant injury in the zone I region may be hidden from inspection of the chest or the mediastinum.
Zone II: Extends from the cricoid to the angle of the mandible. Includes Carotid and vertebral arteries, jugular veins, pharynx, larynx, trachea, esophagus, and cervical spine and spinal cord.
* Most carotid artery injuries are associated with zone II injuries.
Zone III: Extends from angle of mandible to base of skull. The salivary and parotid glands, esophagus, trachea, vertebral bodies, carotid arteries, jugular veins, and major nerves (including cranial nerves IX-XII), traverse this zone. Injuries in zone III can prove difficult to access surgically.
Clinical Pearls:
Follow ATLS: Airway can be very tough and can rapidly deteriorate.
A – Airway. May be distorted, needs to be atraumatic. +/- Indirect Visualization. High suspicion for a laryngeal injury may prompt a surgical airway
B – Consider that Zone I injuries may breach the chest cavity and concern for pneumothorax and/or hemothorax
C – Control bleeding with direct pressure. If not possible consider balloon tamponade (eg. With Foley). Never blindly clamp a vessel. DO NOT remove objects protruding from the neck in the ED. Large bore IV’s X 2. Limit probing of wound
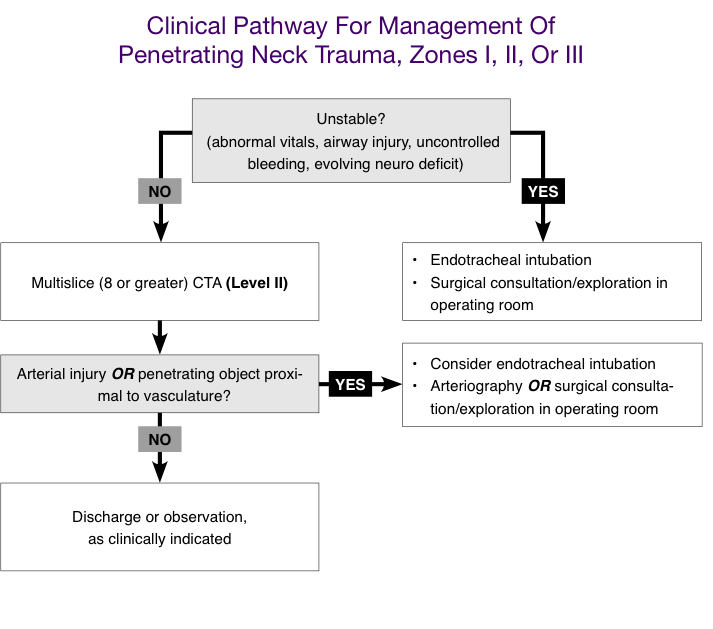
Identify Unstable Patients: include those with clear airway injury (ie. Air bubbling through wound), hemodynamic instability, uncontrolled bleeding, or evolving neurological deficit
CTA can be considered as the initial diagnostic study of choice in penetrating trauma to the neck of ALL ZONES
Cervical spine immobilization is not necessary in penetrating trauma to the neck without evidence of neurological deficit.
Have a HIGH Suspicion for Esophageal Injuries by getting an Esophagoscopy/Esophagography. Bleeding from the mouth, drooling, and subcutaneous emphysema are all suggestive of upper digestive tract injury.
- Missed esophageal injuries have a remarkably high morbidity and mortality (up to 50%) if not detected in the first 24 hours.
Laryngeal Injury: Flexible laryngoscopy
Cervical spine injuries are much less common in penetrating trauma so C collars can be removed in patients without evidence of neurological deficit.
Do not rely on physical examination alone for penetrating neck injuries.
Physical Examination:
Physical examination of the patient should focus on the 3 major organ systems commonly involved in penetrating neck injury: airway, vascular system, and upper digestive tract.
- Evaluation of the airway is focused on the respiratory status of the patient, such as the respiratory rate and signs of airway distress, including dyspnea and stridor. Vocal quality should be noted, and the patient should be questioned about changes in the voice. The neck and upper chest should be palpated for subcutaneous emphysema, and the larynx and trachea should be palpated for tenderness and crepitus. Flexible laryngoscopy, CT imaging, and/or direct laryngoscopy and bronchoscopy may be necessary to fully evaluate suspected airway injuries.
- Injuries to the great vessels of the neck may be obvious on physical examination and may present as an exsanguinating wound or expanding hematoma. A significant vascular injury may be subtle, with findings such as an absent distal pulse, bruit, or isolated neurologic deficit. Suspected vascular injuries can be further evaluated with angiography and exploration.
Imaging Studies:
X-rays: CXR, Soft Tissue Neck. Foreign Body/Free Air
CTA: Initial Diagnostic study of choice. Arteriography
Esophagography: Do not use Barium (use Gastrograffin)
Doppler US: Can look at major Carotids
Jay Khadpe MD
Latest posts by Jay Khadpe MD (see all)
- Morning Report: 7/30/2015 - July 30, 2015
- Morning Report: 7/28/2015 - July 28, 2015
- IN THE STRETCHER INSTEAD OF BESIDE IT - July 22, 2015
- Morning Report: 7/14/2015 - July 14, 2015
- Morning Report: 7/10/2015 - July 10, 2015