Here’s Dr. Paulson with today’s Morning Report!
HYPOKALEMIA
Hypokalemia < 3.5 meq/L
Moderate < 3 meq/L
Severe <2.5 meq/L
Up to 20% admitted pts hypokalemic, only 4-5% clinically significant, “severe” uncommon.
Presentation:
The history may be vague. Often asymptomatic, or symptoms reflect underlying cause.
Think about it with group of sxs involving GI, renal, musculoskeletal, cardiac, and nervous systems.
Common symptoms include the following:
- Palpitations
- Skeletal muscle weakness or cramping, paralysis, paresthesias
- Abdominal cramping, constipation, nausea or vomiting
- Polyuria, nocturia, or polydipsia
- Psychosis, delirium, or hallucinations, depression
Etiology:
- Malnutrition or decreased dietary intake, parenteral nutrition
- Renal losses
- Renal tubular acidosis
- Hyperaldosteronism
- Magnesium depletion
- GI losses
- Vomiting or nasogastric suctioning
- Diarrhea (enemas or laxative use – iatrogenic or psych)
- Medication
- Diuretics** (most common cause)
- Steroids
- Theophylline
- Aminoglycosides
- Transcellular shift
- Beta-adrenergic agonists
- Insulin
- Alkalosis
- Periodic paralysis, thyrotoxicosis
Workup
- Magnesium: levels are unreliable and usually don’t change management, since these pts almost always have concurrent hypomagnesemia and should be treated empirically.
- BUN/Cr
- Glucose, Ca, and/or Phos level if coexistent electrolyte disturbances are suspected.
- Consider digoxin level – hypokalemia can potentiate digitalis-induced arrhythmias.
- Consider ABG: alkalosis can cause transcellular shift
- Electrocardiography
- Long PR interval (increased amp and width of P waves)
- T-wave flattening or inverted T waves
- ST depressions
- Prominent U waves (best seen in precordial leads). Apparent long QT (fused TU)
- Freq PACs and PVCs, AFib, AFlutter
- VT, VF, and TdP
- Thyroid screening studies – TSH, free T3, and free T4 in pts with tachycardia
Treatment: After ABCs…
>2.5 – PO
<2.5 – both PO and IV
Every 10 meq given, K increase serum level by 0.1meq/L
(Consider giving Mag)
Potassium Chloride : PREFERRED AGENT
–Most patients with hypokalemia and acidosis are also chloride depleted
–Raises serum potassium at a faster rate
–Available as salt substitute, liquid, slow release tablet or capsule, and IV
Oral: 40meq tid-qid, IV: Peripheral line 10meq/hr (never more than 20meq/hr) – phlebitis, pain
Potassium Bicarbonate/Citrate/Acetate:
–can be used in patients with hypokalemia and metabolic acidosis
Potassium Phosphate:
–Rarely used (Fanconi syndrome with phosphate wasting)
Treat underlying cause…
T wave inversion and prominent U waves in hypokalemia
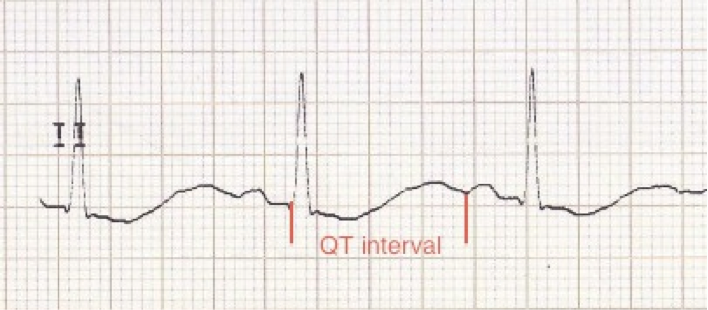 Apparent long QT interval with hypokalaemia (actually T-U fusion)
Apparent long QT interval with hypokalaemia (actually T-U fusion)
Jay Khadpe MD
Latest posts by Jay Khadpe MD (see all)
- Morning Report: 7/30/2015 - July 30, 2015
- Morning Report: 7/28/2015 - July 28, 2015
- IN THE STRETCHER INSTEAD OF BESIDE IT - July 22, 2015
- Morning Report: 7/14/2015 - July 14, 2015
- Morning Report: 7/10/2015 - July 10, 2015


1 comment for “Morning Report: 2/26/13”