Thanks for all the responses and sorry for the delay in posting this answer. Ritchie hit it right on the head. The patient was diagnosed with West Nile Encephalitis. The WNV PCR eventually came back positive. While the diagnosis was not made in the emergency department, the treating physician had viral encephalitis at the top of his differential after seeing the CSF results.
Lets review the imaging:
The CT scan for this patient was relatively normal. Looking at the sinuses we can see some mucosal thickening and fluid in the left sphenoid and frontal sinuses. These are likely incidental findings. The MRI was obtained while the patient was still in the emergency department but admitted to the ICU. Before we go into the specific findings of the MRI lets go over some MRI basics, since this is not an imaging modality that we typically read ourselves.
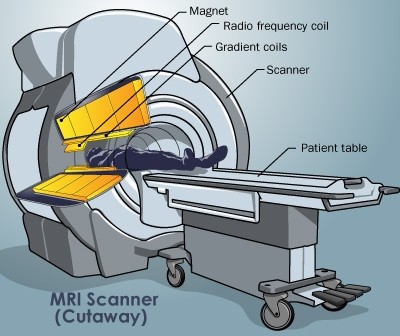
The MRI has basically 3 parts: a superconducting magnet, radiofrequency coils and gradient magnets. The superconducting magnet is always on and causes all of the hydrogen atoms in your body to align either with or against the magnetic field. The alignment of the atom is called “spin”. Ideally, exactly half of the atoms have “positive” spin and the other half have “negative” spin. However, there are always a few outliers – hydrogen atoms that are not balanced by another atom. It’s these atoms that the MRI uses to generate an image. The next step is a radiofrequency pulse directed at the specific area of interest (slice). The pulse is only absorbed by the unbalanced hydrogen atoms and once the pulse is turned off, the atoms return to their original spin state and release energy. Roughly, the energy released corresponds to a frequency which gives us information about the tissue and helps to generate an image.
Some of the common MR images obtained are T1, T2 and FLAIR. These images are generated based on how the hydrogen atoms react to the RF pulse. The result is that T1, T2 and FLAIR images give us different information about the tissue of interest.
- T1
- Bright – Fat, Melanin, Hemorrhage, Protein-rich fluid, Gadolinium
- Dark – CSF, Water (edema, tumor, infarct, infection, inflammation, chronic hemorrhage), Calcification
- White matter is brighter than Gray matter
- T2
- Bright – Water (edema, tumor, infarct, infection, inflammation, chronic hemorrhage)
- Dark – Calcifications, Fibrous tissue, Iron, hemosiderin, melanin, methemoglobin, Protien rich fluid
- Gray matter is brighter than White matter
- FLAIR – T2 images with the signal from free water removed – Bright = PATHOLOGY
- Diffusion Weighted Imaging – Specifically looks for infarcts which show up as bright spots
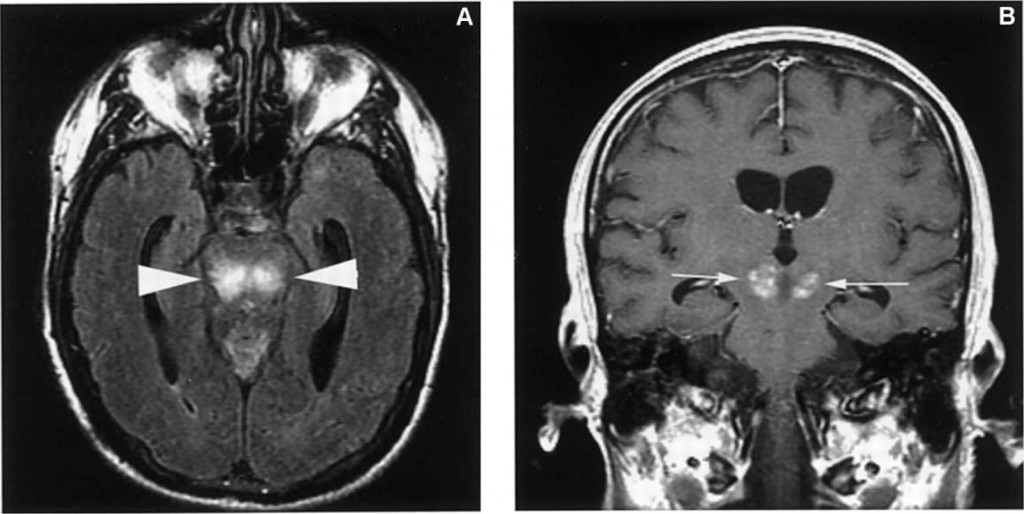
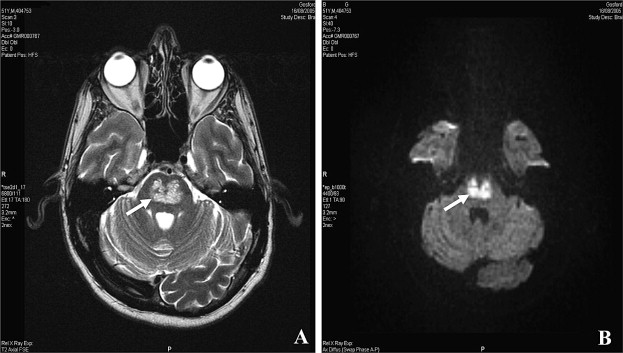
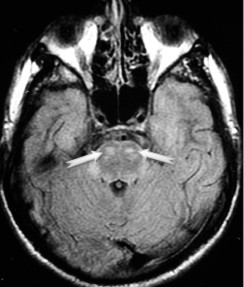
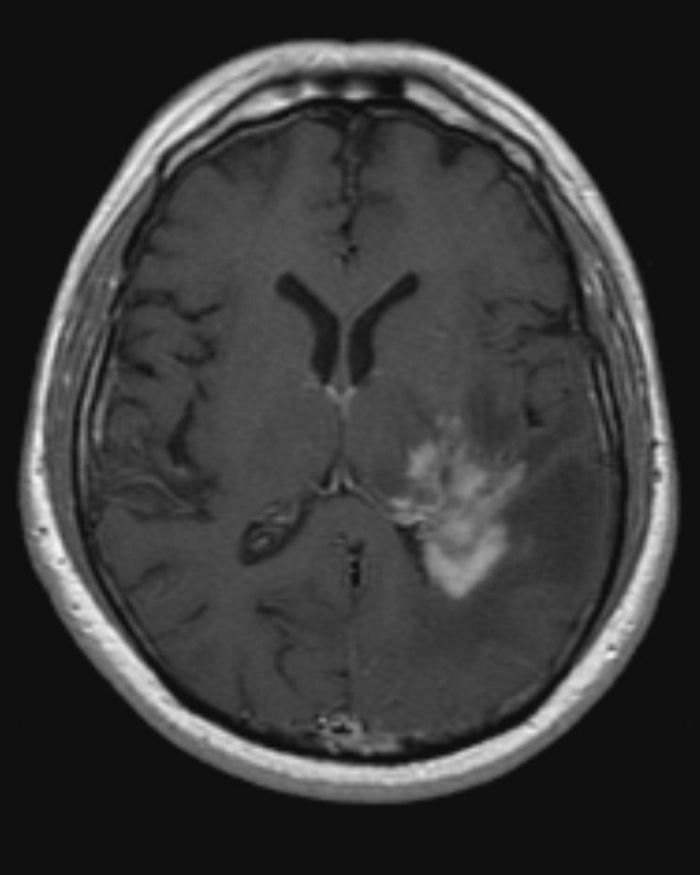
So back to our patient. The first MRI image shows white matter as dark and grey matter as bright. This tells you its a T2 image. However, CSF is usually bright in a T2 image while in our image the CSF is dark. The CSF is mostly free water so these images represent FLAIR. In interpreting these images we can see that there is significant enhancement in the thalami extending into the cerebral peduncles bilaterally.
In the second video we see the T1 images and again we enhancement of the thalami and cerebral peduncles bilaterally. However, pathology in T1 images is usually dark (with the exception of free water). The fact that there is uptake in an area also identified by FLAIR suggests we did something to that area to highlight it. We can deduce that this T1 scan was done with gadolinium contrast. This contrast leaks out of the capillaries in areas of edema and inflammation and highlights pathology.
Finally, diffusion weighted imaging (DWI) did not show any signs of an infarct.
DDX
West Nile Virus
Based on the clinical history and laboratory tests, viral encephalitis was at the top of our differential. As Ritchie stated, the protein in the CSF and MRI findings support this diagnosis. Typical MRI findings of WNV infection include hyperintensity in the basal ganglia, caudate, thalami, brainstem and spinal cord as seen here.
WNV is transmitted by the bite of an infected mosquito. Incubation period ranges from 2-14 days. Only about 20-40% of patients infected with WNV become symptomatic. The usual presentation is that of a viral syndrome with fever, headache, myalgias lasting 3-6 days. It can present with a maculopapular rash in up to 50% of patients but usually those with neuroinvasive disease do not have a rash.
In some patients, WNV can progress to neuroinvasive disease including meningitis and encephalitis. Encephalitis is more common in elderly, alcoholic or diabetic patients and can range from mild confusion to coma and death. Given the location of involvement on MRI clinical exam features are predictable, including extrapyramidal symptoms, tremor, myoclonus (usually upper extremities) and parkinsonian features (rigidity, instability, bradykinesia). The diagnosis is made by isolating WNV IgM or DNA in CSF samples. Treatment is primarily supportive care although some weak evidence exists for the use of interferon in severe cases. Ribavirin has not been proven effective.
Osmotic Demyelination Syndrome
Another clinical entity that can have a similar presentation and MRI findings is osmotic demyelination syndrome. ODS occurs with rapid correction of hyponatremia in patients who are chronically hyponatremic. Symptoms are usually delated 2-6 days after the correction. Patients develop dysarthia, dysphagia, paresis, lethargy, confusion, obtundation and coma. In severe cases patients become “Locked In” – awake but unable to communicate.
ODS is thought to occur because patients that are chronically hyponatremic lose osmotically active substances from the brain. These substances protect against cerebral edema. Once the hyponatremia is corrected, the brain volume shrinks which leads through demyelination. Risk factors for ODS include the level of hyponatremia (<120), duration of hyponatremia (>3 days), and rapidity of correction (>10meq/24hr). Prevention of ODS involves treating the underlying cause of hyponatremia (dehydration, SIADH, adrenal insufficiency) as well as ensuring that the hyponatremia is corrected at a rate of about 0.5meq/hr. Various calculators are available online to help determine the correct fluids and rate to safely correct hyponatremia – http://www.medcalc.com/sodium.html.
Toxic Inhalation of Toluene
Tolune is a hydrocarbon that has a high lipid solubility. It is found in many glues, cement, markers, paints and paint thinner. It is inhaled and crosses membranes easily and given the high lipid content of neurons can cause significant CNS toxicity. Toluene acts on glutamate and GABA receptors on neurons to produce CNS depression. Its CNS effects include slurred speech, ataxia, disorientation, headache, hallucinations, agitation and seizures. Cardiac affects include arrhythmias typically prolonging the QT. Toluene also causes metabolic acidosis, muscle weakness, rhabdomyolysis and birth defects. Case reports have shown that toluene inhalation can result in MRI findings including high intensity on T2 images of the internal capsule, brainstem and cerebrum. Treatment of toluene inhalation is mainly supportive by providing oxygen to correct hypoxia and standard ACLS management of arrhythmias.
Malignancy – Primary CNS Lymphoma
 Primary CNS lymphoma is one of the AIDS defining malignancies. It is thought to occur in conjunction with EBV infection and accounts for 15% of non-hodgkins lymphomas in HIV patients. It can occur in non-HIV infected patients although it is more rare. CD4 counts of patients with PCL are typically lower than 50. Patients can present with focal or non-focal signs and symtoms and is usually subacute (presenting over 1-3 months). Symptoms include confusion, lethargy, memory loss, hemiparesis, aphasia and seizures. Diagnosis is made by finding lesions on CT or MRI and subsequently excluding toxoplasmosis infection by using CSF cytology, Toxo IgG/IgM, empiric antibiotics, EBV DNA assays and brain biopsy if needed. PCL can cause lesions anywhere in the CNS that can be isodense and hyperdense on MR imaging. Up to half of patients with PCL have multiple lesions at the time of presentation. Treatment includes chemotherapy agents (methotrexate) and HAART.
Primary CNS lymphoma is one of the AIDS defining malignancies. It is thought to occur in conjunction with EBV infection and accounts for 15% of non-hodgkins lymphomas in HIV patients. It can occur in non-HIV infected patients although it is more rare. CD4 counts of patients with PCL are typically lower than 50. Patients can present with focal or non-focal signs and symtoms and is usually subacute (presenting over 1-3 months). Symptoms include confusion, lethargy, memory loss, hemiparesis, aphasia and seizures. Diagnosis is made by finding lesions on CT or MRI and subsequently excluding toxoplasmosis infection by using CSF cytology, Toxo IgG/IgM, empiric antibiotics, EBV DNA assays and brain biopsy if needed. PCL can cause lesions anywhere in the CNS that can be isodense and hyperdense on MR imaging. Up to half of patients with PCL have multiple lesions at the time of presentation. Treatment includes chemotherapy agents (methotrexate) and HAART.
Conclusion
When looking at the MRI findings of our patient without knowing the history, the differential diagnosis can include a variety of entities as discussed above. On the basis of MR findings alone PCL is less likely given the picture of bilateral lesions in the thalami and brainstem. However, the others all have a similar appearance and can have a similar clinical presentation. When the history and laboratory find are added it becomes clear that WNV was the most likely diagnosis.
References:
http://www.howstuffworks.com/mri.htm
http://www.radpod.org/2007/08/06/primary-cns-lymphoma/
UpToDate – AIDS-related lymphomas: Primary central nervous system lymphoma
UpToDate – Inhalant abuse in children and adolescents
UpToDate – Osmotic demyelination syndrome and overly rapid correction of hyponatremia
UpToDate – Clinical manifestations and diagnosis of West Nile virus infection
Twardowschy, Carlos Alexandre et al. Optic neuritis due to solvent abuse. Arq. Neuro-Psiquiatr. 2008, vol.66, n.1, pp. 108-110. ISSN 0004-282X.
Huq, S. et al. Osmotic demyelination syndromes: central and extrapontine myelinolysis. Journal of Clinical Neuroscience 14 (2007) pp. 684-688.
Hong, David S. et al. West Nile Encephalitis in 2 Hematopoietic Stem Cell Transplant Recipients. Clin Infect Dis October 15, 2003vol. 37 no. 8 1044-1049
nchristopher
Latest posts by nchristopher (see all)
- What’s wrong with this picture? – Answer - September 11, 2013
- What’s wrong with this picture? - August 21, 2013
- EKG Case 8 – Answer - July 16, 2013
- EKG Case 8 – All that wheezes - June 19, 2013
- EKG Case 7 Answer - June 19, 2013