Here’s Dr. Caputo with today’s Morning Report!
Mastering the Tympanic Membrane
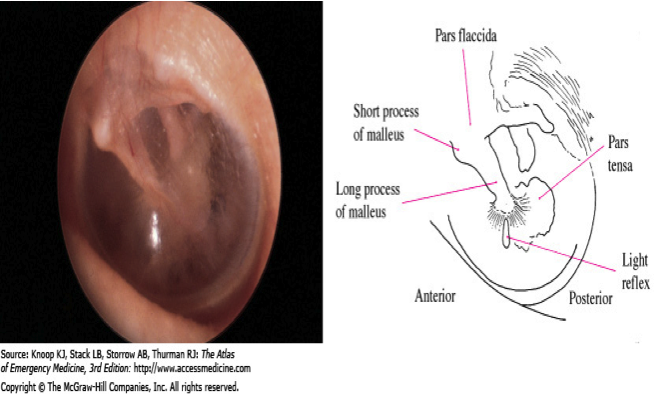
Normal Anatomy:
Acute Otitis Media: Highest risk 2 months – 6 years. Acute inflammation and effusion of the middle ear. Otoscopy should focus on color, position, translucency, and mobility of the TM. AOM causes the TM to appear dull, erythematous or injected, bulging, and less mobile. The light reflex, normal TM landmarks, and malleus become obscured.
Bullous Myringitis: Bullous myringitis is a direct inflammation and infection of 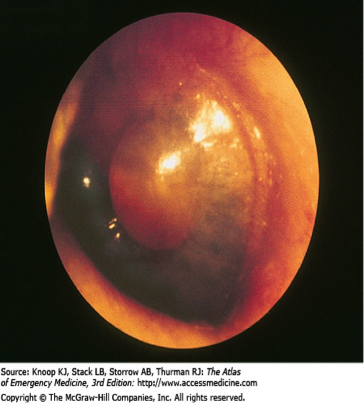 the tympanic membrane (TM) secondary to a viral or bacterial agent. Usually preceded by URI. Vesicles or bullae filled with blood or serosanguinous fluid on an erythematous TM are the hallmark. Frequently a concomitant otitis media with effusion is noted. Common bacterial agents are Mycoplasma pneumoniae, Streptococcus pneumoniae, and Haemophilus influenzae. Treatment: Although most episodes resolve spontaneously, many physicians prescribe antibiotics such as Bactrim or a macrolide. Warm compresses, topical or strong systemic analgesics, and oral decongestants may provide symptomatic relief. Referral is not necessary in most cases unless rupture of the bullae is required for pain relief.
the tympanic membrane (TM) secondary to a viral or bacterial agent. Usually preceded by URI. Vesicles or bullae filled with blood or serosanguinous fluid on an erythematous TM are the hallmark. Frequently a concomitant otitis media with effusion is noted. Common bacterial agents are Mycoplasma pneumoniae, Streptococcus pneumoniae, and Haemophilus influenzae. Treatment: Although most episodes resolve spontaneously, many physicians prescribe antibiotics such as Bactrim or a macrolide. Warm compresses, topical or strong systemic analgesics, and oral decongestants may provide symptomatic relief. Referral is not necessary in most cases unless rupture of the bullae is required for pain relief.
Cholesteatomas are collections of desquamating stratified squamous 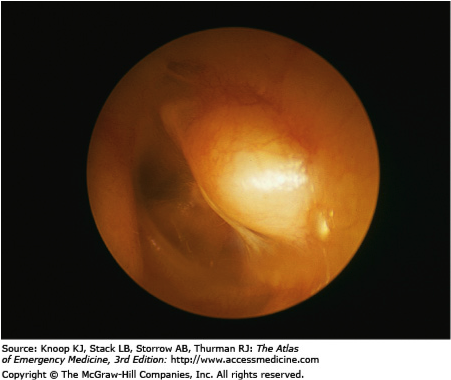 epithelium found in the middle ear or mastoid air cells. Congenital cholesteatomas are most frequently found in children and young adults. Acquired cholesteatomas originate from perforations of the tympanic membrane. Cholesteatomas can be locally destructive of the middle ear ossicles and tympanic membrane through the production of collagenases. They may also erode into the temporal bone, inner ear structures, mastoid sinus, or posterior fossa dura. Delays in treatment can lead to permanent conductive hearing loss or infectious complications. Therefore, may require surgical excision and ENT referral.
epithelium found in the middle ear or mastoid air cells. Congenital cholesteatomas are most frequently found in children and young adults. Acquired cholesteatomas originate from perforations of the tympanic membrane. Cholesteatomas can be locally destructive of the middle ear ossicles and tympanic membrane through the production of collagenases. They may also erode into the temporal bone, inner ear structures, mastoid sinus, or posterior fossa dura. Delays in treatment can lead to permanent conductive hearing loss or infectious complications. Therefore, may require surgical excision and ENT referral.
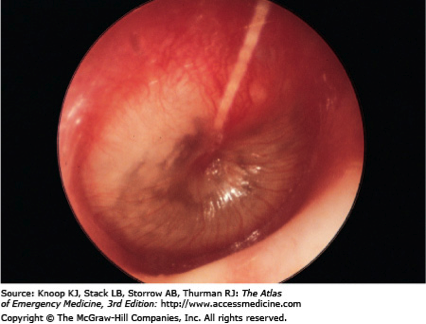
TM Perforation: Antibiotics and irrigation do not improve the rate or  completeness of healing unless the injury is associated with OM. Systemic antibiotics should be reserved for perforations associated with OM, penetrating injury, and possibly water-sport injuries
completeness of healing unless the injury is associated with OM. Systemic antibiotics should be reserved for perforations associated with OM, penetrating injury, and possibly water-sport injuries
Patients are instructed to avoid allowing water to get into the ear while the perforation is healing and to return if symptoms of infection appear. Even though nearly 80% of all TM perforations heal spontaneously, all TM perforations should be referred to an otolaryngologist for follow-up for possible myringoplasty.
Otitis Externa: or “swimmer’s ear,” is an inflammation and infection (bacterial or 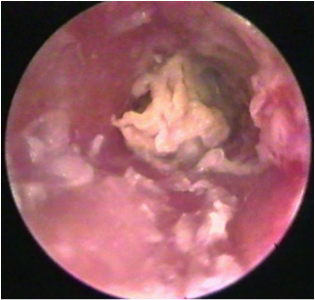 fungal) of the auricle and external auditory canal. Saline irrigation and suctioning is recommended to thoroughly evaluate the EAC. Topical antibiotic suspensions containing polymyxin, neomycin, and hydrocortisone or ciprofloxacin with ear wicks are effective
fungal) of the auricle and external auditory canal. Saline irrigation and suctioning is recommended to thoroughly evaluate the EAC. Topical antibiotic suspensions containing polymyxin, neomycin, and hydrocortisone or ciprofloxacin with ear wicks are effective
Reference: Knoop KJ, Stack LB, Storrow AB, Thurman RJ: The Atlas of Emergency Medicine, 3rd Edition: http://www.accessmedicine.com
Jay Khadpe MD
Latest posts by Jay Khadpe MD (see all)
- Morning Report: 7/30/2015 - July 30, 2015
- Morning Report: 7/28/2015 - July 28, 2015
- IN THE STRETCHER INSTEAD OF BESIDE IT - July 22, 2015
- Morning Report: 7/14/2015 - July 14, 2015
- Morning Report: 7/10/2015 - July 10, 2015
