 Here’s this weeks EKG case! Thanks to Niki for submitting the case!
Here’s this weeks EKG case! Thanks to Niki for submitting the case!
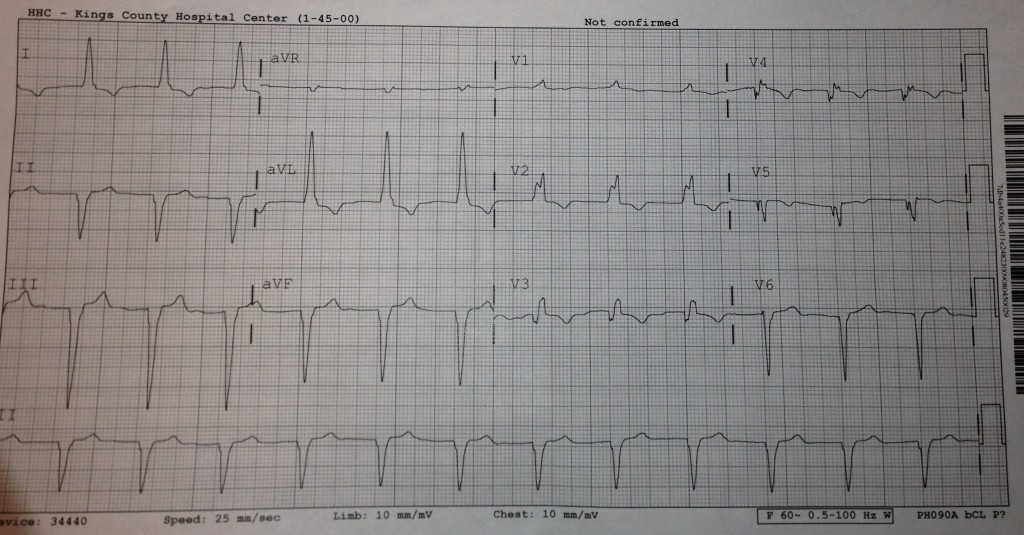
This week we’ll try to not just interpret the EKG but use it in addition to other clinical findings to bring us to our diagnosis.
59yo F presents with a chief complaint of chest pain and shortness of breath. Her triage vitals are 157/102, 84, 20, 97.4, 94% sat on RA.
Her only hx that she can recall is HTN and arthritis. She is visiting from the West Indies. There are no prior EKGs available.
Please reply below with your interpretation of the EKG. Additionally, you can ask for further history, exam findings, labs, imaging, ultrasound… etc… How would you work up this patient? What studies are essential? What is your differential?
The views expressed on this blog are the author's own and do not reflect the views of their employer. Please read our full disclaimer here. Any references to clinical cases refer to patients treated at a virtual hospital, Janus General Hospital.
The following two tabs change content below.


nchristopher
Latest posts by nchristopher (see all)
- What’s wrong with this picture? – Answer - September 11, 2013
- What’s wrong with this picture? - August 21, 2013
- EKG Case 8 – Answer - July 16, 2013
- EKG Case 8 – All that wheezes - June 19, 2013
- EKG Case 7 Answer - June 19, 2013

2 comments for “Rhythm Nation: Not Just the EKG”