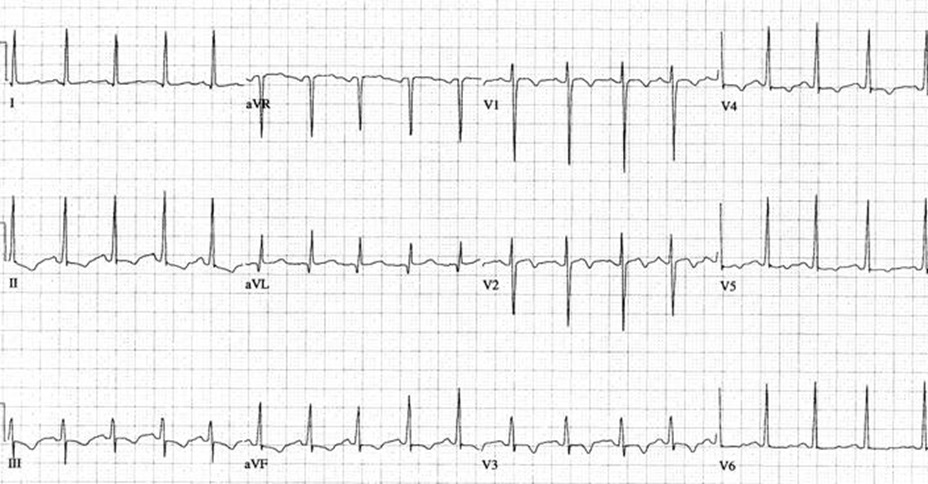
 Thanks for the responses on our last EKG case. To review, the patient was a 24 YO woman with PMH of asthma presenting with chest tightness, shortness of breath and wheezing. Her exam was significant for B/L wheezes. There was no LE swelling. Something about her presentation doesn’t feel right and you get the above EKG.
Thanks for the responses on our last EKG case. To review, the patient was a 24 YO woman with PMH of asthma presenting with chest tightness, shortness of breath and wheezing. Her exam was significant for B/L wheezes. There was no LE swelling. Something about her presentation doesn’t feel right and you get the above EKG.
Further information… She has no PMH other than asthma. She has no family history. No recent travel, no OCP use, no FH of DVT/PE. She is not fat, no smoking history, no fever or cough. No hx of TB or recent viral illness. Her CXR was clear and showed no cardiomegaly.
EKG Interpretation
Sinus tachycardia, rate 114, normal axis, normal intervals, T wave inversions in V1-V4 and II,III, aVF. No ST segment elevation or depression. No signs of atrial or ventricular hypertrophy. P waves are all upright in the inferior leads and for the most part are consistent morphology so its unlikely to be MAT
Disposition
This patient, on further questioning was found to have LMP 8 wks ago. The pregnancy was confirmed with positive UCG and ultrasound showing IUP. After further testing the patient was found to have a saddle embolus and a DVT!
EKG changes in the setting of pulmonary embolism
The classic EKG changes we see for pulmonary embolism are NON-SPECIFIC. Most commonly the patient will just have sinus tachycardia! In rare cases you do see the dreaded S1Q3T3 (S wave in 1, Q wave and TWI in lead 3). However, even this finding is not specific for PE, it is merely a sign of right heart strain. So your patients with end stage COPD or pulmonary hypertension with cor-pulmonale will usually have these EKG changes as well.
In this case, our patient had TWI in the inferior as well as anteroseptal leads. While these T wave changes can be non-specific, there is some literature that states the combination of anterior and inferior TWI is sensitive and specific for PE. Kosuge et al. in the European Heart Journal studied patients with TWI in V1-V4 and found that TWI in lead III and lead V1 had a 90% sensitivity and 97% specificity for pulmonary embolism. The combination of these two leads was shown to be useful at differentiating ACS from PE. The same group has another paper suggesting that the number of TWI in patients with pulmonary embolism has prognostic significance. Patients with TWI in 7 or more leads had higher rates of in hospital complications as well as right heart failure on echo. Its important to note though, that this was a very small study.
There are a whole bunch of other EKG changes that can be seen in pulmonary embolism – including RBBB, poor R wave progression, atrial tachyarrhythmias, R wave in V1 and many more. However, the findings in our EKG have been shown to be the most specific for PE in the literature.
Pulmonary embolism is one of the most difficult diagnoses to make in the emergency department. That’s one of the reasons we have so many rules and guidelines to help decide how to approach patients in which PE is on the DDx. If you think the patient is low risk (as in your pretest probability for PE is < 15%), you can try seeing if they pass the PERC rule. This gives them a 2% probability of having an embolism.
If they don’t pass the PERC you can try the Wells Criteria. Low risk patients with 1 point have about a 1.3% incidence. Moderate risk (2-4 points) have about have about a 16% risk and high risk > 4 have a 28% risk. However, since part of the wells criteria is deciding if PE is as likely as any other diagnosis, it is very easy to get scores > 4. In patients that are low or moderate risk, a negative D-dimer may be enough to rule out PE, but those patients that are moderate risk usually require a VQ scan or a CT angiogram.
What do you think? How do you approach patients when PE is on the differential?
nchristopher
Latest posts by nchristopher (see all)
- What’s wrong with this picture? – Answer - September 11, 2013
- What’s wrong with this picture? - August 21, 2013
- EKG Case 8 – Answer - July 16, 2013
- EKG Case 8 – All that wheezes - June 19, 2013
- EKG Case 7 Answer - June 19, 2013
