Thanks to those who participated. That’s Dr. Dan Zeccola. And, Dr. Dan Zeccola.
Dan did a fantastic job of running through the findings that can help distinguish ventricular tachycardia vs a rhythm of supraventricular origin. I also recommend you check out lifeinthefastlane.com, which is chock full of EM and critical care pearls. It’s review of VT vs SVT with aberrancy is spot-on awesome.
Without repeating Dan’s review, I wanted to offer a few other helpful discriminators of VT vs SVT. Before scrutinizing an ECG, certain historical factors increase the probability of VT:
- Age over 35
- Hx of previous MI
- Hx of structural heart disease
- Hx of ischemic heart disease
- Hx of cardiomyopathy
- Hx of familial sudden cardiac death
ECG findings that make VT more likely:
- AV dissociation, capture beats, fusion beats are pathognomonic for VT
- Extremely-wide complexes (>160ms)
- Absence of typical RBBB or LBBB morphology
- RsR’ with left bunny ear taller than the right (RBB-ish, but different)
- Precordial-concordance (V1-V6 all have same vector)
- NW axis
- Brugada’s Sign: time from onset of QRS to S-wave nadir is >100ms
- Josephson’s Sign: Notching near the S wave nadir
There are formal algorithms for working up wide-complex tachycardia, ie. Brugada’s criteria, which is beyond the scope of this review.
While the above are useful for the evaluation of stable wide-complex tachycardia, they presume one thing that Dr Zeccola did not mention. Ventricular Tachycardia is super-regular. This rhythm is fast and wide. It is so fast, in fact, that it appears regular. But upon close inspection, it is not.
I’ll be honest; I knew the case particulars and the patient’s history and still missed the irregularity. This patient had a history of WPW. Now, anyone with an accessory pathway is prone to dysrhythmias, especially AVRT, which is regular and fast and can be either wide- or narrow-complex depending on how the impulses travel through the AV node. But they are also prone to the DO NOT MISS diagnosis, a fib with WPW. Missing this possibility is how you kill an otherwise stable-ish patient. (AV nodal agents that slow nodal transmission can drive the atrial impulses down the accessory pathway fast enough to induce v fib.)
So when should you suspect a fib with WPW. Obviously, it helps to know that the patient has WPW, but this isn’t always the case. Extremely fast rates, >180, should make you think about it. QRS complexes of varied morphologies should make you think about it. And irregularity.
The differential for a wide, fast, and irregular rhythm is short: atrial fibrillation with aberrancy, atrial fibrillation with WPW, and polymorphic ventricular tachycardia. That’s a touch over-simplified, though. Any irregularly irregular supraventricular rhythm that’s aberrantly conducted fits the bill, including MAT with aberrancy or a flutter with variable block, for instance.
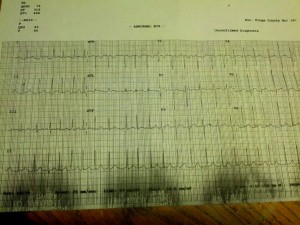
To wrap-up the case, this was a mid-30s gentleman, with a history of WPW. He was referred from pulmonary clinic (he also had sarcoid) with a heart rate of 210. The initial ECG recorded is above. We missed the irregularity and I made the argument that this was AVRT, as it was so “regular.” An astute CCT attending prevented me from giving AV nodal agents and instead we administered the correct medication, procainamide, 1g over 1 hour.
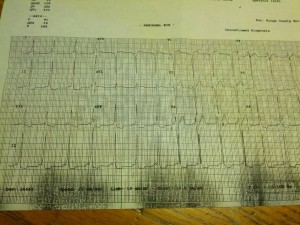
The following ECG’s were recorded over the next hour.
The first shows a fast, narrow-complex irregularly irregular rhythm. Now in the 140s, there is no uncertainty about the irregularity here. This is a fib.
Over the next few minutes, he developed this rhythm: sinus, regular, slow with distinct delta waves.
In short, always keep a fib with WPW in your head when evaluating a wide and fast rhythm. And do no harm.
Amazing case. Thanks to Drs Silverberg and Sterling for their wisdom and restraint. And Thanks to Lifeinthefastlane.com.
jfreedman
Latest posts by jfreedman (see all)
- Less is More - April 13, 2015
- Don’t just do something, stand there. - January 19, 2015
- All pressure is created equal - September 15, 2014
- The “Soft” Code - June 23, 2014
- 6/25 Adult Journal Club - June 16, 2014

1 comment for “Case 9 – Answer and Discussion”