This is a fictitious patient seen at a fictitious hospital called Janus General. Don’t believe me? I’m on staff there – see
65 yo F pmhx HTN/DM presents with worsening abdominal pain for 2 days. Pain is generalized, 10/10, no radiation, previously intermittent, but is now constant for hours. No known exacerbating/alleviating factors.
Eating less, but still drinking. Last BM yesterday – watery, non-bloody diarrhea x 2. +Nausea, vomiting, NBNB x 1 this AM.
ROS: + subjective fevers/chills without measured temp, +mild pedal edema x few days
ROS: no joint pain, no red or black stool, no dysuria/frequency/urgency, no trauma, no back pain, no weakness or numbness, no recent travel or URI, no recent antibiotic use or hospitalizations, no neck stiffness, sick contacts.
Denies toxic habits
No previous surgeries.
VS HR 155, BP 170/60, RR 23, Temp (oral) 100.3, O2sat 99% on RA
PE agitated, uncomfortable, appears to have active abdominal pain
CV: tachycardic, 2/6 systolic murmur, no g/r
Pulm: CTAB w/o w/r/r
Abd: soft, nt,nd.
Neuro exam diff as pt uncooperative. No obvious neuro deficitis.
No meningismus/rashes
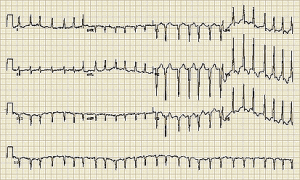
Please see the attached EKG
Before looking at the links below, please think about your differential diagnosis and what interventions/tests you think the patient needs. Bonus points if you put this in your final answer.
Medications/actions
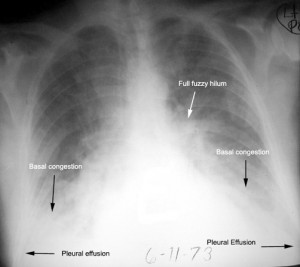
Initial Imaging
Labs
After reviewing the lab results and presentation what must be done?
For the prize of the week: After reviewing the above presentation, what additional test do you want and what is the diagnosis? Please describe an appropriate treatment plan including disposition.
By Dr. Andrew Grock
andygrock
- Resident Editor In Chief of blog.clinicalmonster.com.
- Co-Founder and Co-Director of the ALiEM AIR Executive Board - Check it out here: http://www.aliem.com/aliem-approved-instructional-resources-air-series/
- Resident at Kings County Hospital
Latest posts by andygrock (see all)
- A Tox Mystery…. - May 26, 2015
- Of Course, US Only for Kidney Stones… - May 18, 2015
- Case of the Month 11: Answer - May 12, 2015
- Too Classic a Question to Be Bored Review - May 5, 2015
- Case of the Month 11: Presentation - May 1, 2015

3 comments for “Case of the Month #1 – Presentation, 7/4/14”