Hemorrhage is one of the leading causes of mortality in trauma patients: responsible for approximately 30-40% of deaths overall and 50% of deaths within the first 24-hours post-trauma. Wow. That’s a great deal. So let them have blood? Well… not so simple. First, there is the poorly understood “coagulopathy of trauma,” due to the body’s intense response to activate coagulation pathways to stop bleeding; 25-35% of trauma patients present with coagulopathy, which is associated with a 7x increase in mortality. Next, once fluid resuscitation and massive transfusion protocols are activated, a dilutional coagulopathy that comes into play. So, as you can imagine, the body’s most important defense to stop bleeding becomes quite complicated, leaving the resuscitating physician guessing on a patient’s blood product requirements.
Studies have shown INR, PT, PTT may be inadequate in determining the trauma patient’s blood product requirement. There has been great interest in thromboelastography (TEG), a coagulation test that can assess clot strength, platelet function and fibrinolysis, as an adjunct to help guide resuscitation. TEG is a viscoelastic hemostatic assay that can be used as a bedside point-of-care test (takes about 30 minutes) to assess a trauma patient’s acute coagulopathy, allowing the physician to replete based on the body’s hemostatic needs, leading to a safer, more efficient and cost-effective technique in blood product replacement. Additionally, cohort studies show that use of this test decreases mortality in trauma patients!
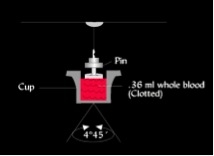
How does it work exactly? 0.3 cc of whole blood is placed in a cup heated to 37 degrees Celsius. The cup is gently rotated back and forth at a set speed around a stationary pin attached to a torsion wire in the center of the cup. Fibrin begins to form between the torsion wire and wall of the cup. The speed and strength of the clot are converted into an electrical signal via a mechanical-electrical transducer that is then analyzed by a computer and depicted in a graphic representation
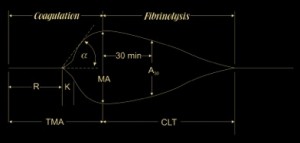
The graph looks something like this:
Where,
– R is the reaction time: time from start of test to initial fibrin formation.
– K is the kinetics: time taken to achieve a certain level of clot strength
– Alpha is the angle: measures the speed at which fibrin builds up and cross- linking takes place, ie- rate of clot formation
– TMA is the time to maximum amplitude
– MA is the maximum amplitude
– A30 or LY30 is the amplitude at 30 minutes, decrease in amplitude at 30 minutes post-MA gives measure of the degree of fibrinolysis
– CLT is clot lysis time
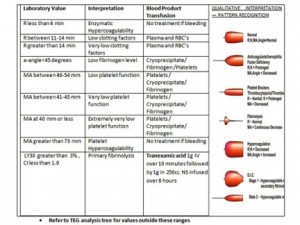
These numbers can be interpreted to guide blood product transfusion:
So, all in all, TEG has peaked the interest of trauma physicians and has great potential in becoming a widely used tool in guiding trauma resuscitations in hemorrhaging patients.
References:
- Johansson PI, Stissing T, Bochsen L, Ostowski SR. Thromboelestography and thromboelastometry in assessing coagulopathy in trauma. Scandinavian Journal of Trauma. 2009, 17:45. http://www.sjtrem.com/content/17/1/45
- Hess JR, Brohi K, Dutton RP, et al. The coagulopathy of trauma: a review of mechanisms. J Trauma. 2008;65(4):748-754.
- Chambers LA, Chow SJ, Shaffer LE. Frequency and characteristics of coagulopathy in trauma patients treated with a low- or high-plasma-content massive transfusion protocol. Am J Clin Pathol. 2011 Sep;136(3):364-70.
- Brazzel C. Thromboelastography-guided transfusion Therapy in the trauma patient. AANA J. 2013 Apr;81(2):127-32.
- Plotkin et alA reduction in clot formation rate and strength assessed by thromboelastography (TEG) is indicative of transfusion requirements with penetrating injuries. Journal of Trauma. February 2008 Vol 64(2) pp64-68
- www.uktraumaprotocol.blogspot.com. Accessed July 2014.
- Nickson, C. Thromboelastogram. www.lifeinthefastlane.com. Accessed July 2014.
sadia.hussain
Latest posts by sadia.hussain (see all)
- A Critical Care Frequent Flyer: Stroke - October 14, 2014
- As if Math Wasn’t Traumatic Enough… Calculating Injury Severity Scores - October 13, 2014
- Congeal your knowledge on Thromboelastography… Read on! - July 22, 2014
- I Saw the Pediatric Seatbelt Sign and It Opened Up My Eyes… I Saw the Sign. - June 9, 2014
- Trauma Patient, No IV…CT With IO Contrast? - April 13, 2014