Brought to you by Dr. Michelle DiMare
Also titled: US vs H&P
Welcome to yet another exciting installment of our awesome ultrasound blog! For this post, “Name that Tune” rules apply and I challenge you to “name that diagnosis” in 1 number, 1 letter, 1 word and 1 image…
28 F, syncope
Is the patient in the OR yet?
Maybe a few more words and images will help…
Made up Case
A 20 something female is brought over after a witnessed syncopal episode in triage. According to the nurse, who is now just as diaphoretic as the patient, her chief complaint was syncope. You have no vital signs, the patient is perspiring and perseverating and finally blurts out, “I’m 8 weeks pregnant.”
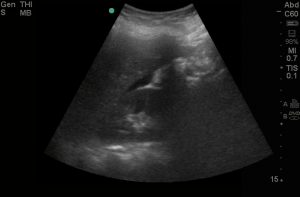
As the nurse goes IV/monitor, grab the sono for a RUQ view.
The above image clearly shows?Until proven otherwise diagnoses this patient has?
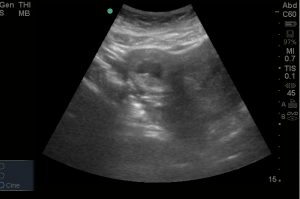
The above further imaging shows?
Ob/Gyn was consulted and the patient was out of the ED in less than 20 minutes.
Ectopic Pregnancy
Early on in our ED education, we are taught that an ectopic pregnancy is a “can’t miss” diagnosis. It accounts for up to 9% of all maternal mortality. However, studies repeatedly find that we can, and do, miss ectopic pregnancy in the ED. In fact, one study demonstrated that 40-50% of ectopic pregnancies were missed on initial presentation. The truth is that this statistic seems high because it takes into account all of the patients with BHCG levels in the discriminate zone and all patients who have normal vital signs, no free fluid in the abdomen and no signs of either ectopic or IUP. These patients are all sent home with return precautions and close follow up. Basically, we suspect they may have an ectopic but even if they do, they don’t need to go to the OR immediately. How then do we find the patients who need to go to the OR?
DO A FAST EXAM!
Even in a stable patient, fluid in the RUQ is a very strong indicator that the patient will need operative intervention. A 2007 study in Academic Emergency Medicine clearly illustrates this. In this study, Moore et al., enrolled 256 patients with suspected ectopic pregnancy. Patients met this criteria simply by being pregnant and having either abdominal pain or vaginal bleeding. All of the patients had both a RUQ view of the FAST exam and a transabdominal pelvic ultrasound. Of these patients, 28 were found to have ectopic pregnancies. Of these, 10 were found to have free fluid in Morison’s pouch by the ED physician and 9 of them went to the OR.
Clearly, the RUQ view does not take the place of a transvaginal ultrasound but this study suggests that adding a standard RUQ view as the initial US view could decrease time to intervention.
Furthermore, while nearly all ED physicians are trained in the FAST exam and have access to a curvilinear or phased array US probe to perform the FAST exam. A much smaller group have access to and are trained in transvaginal ultrasound. In EDs where patients must have their initial assessment and then be sent out of the department for a transvaginal ultrasound, the benefits to a preliminary RUQ view are even more significant.
Hope you enjoyed reading, now go check out those RUQs!!
By Michelle DiMare, MD
Kaplan BC, Dart RG, Moskos M, Kuligowska E, Chun B, Adel Hamid M, et al. Ectopic pregnancy: prospective study with improved diagnostic accuracy. Ann Emerg Med. 1996;28:10–7.
Moore, C., Todd, W.M., O’Brien, E., and Lin, H. Free fluid in Morison’s pouch on bedside ultrasound predicts need for operative intervention in suspected ectopic pregnancy. Acad Emerg Med. 2007; 14: 755–758
andygrock
- Resident Editor In Chief of blog.clinicalmonster.com.
- Co-Founder and Co-Director of the ALiEM AIR Executive Board - Check it out here: http://www.aliem.com/aliem-approved-instructional-resources-air-series/
- Resident at Kings County Hospital
Latest posts by andygrock (see all)
- A Tox Mystery…. - May 26, 2015
- Of Course, US Only for Kidney Stones… - May 18, 2015
- Case of the Month 11: Answer - May 12, 2015
- Too Classic a Question to Be Bored Review - May 5, 2015
- Case of the Month 11: Presentation - May 1, 2015