By Dr. Michelle DiMare
Welcome back and Happy New Year!
While the gallbladder itself and the majority of its pathology are usually considered easily identifiable on basic bedside ultrasound, finding the common bile duct often earns top honors as our nemesis. We must be careful to not fall for a few classic, but potentially serious, gallbladder fakeouts…
Case 1: A 45 year old female presents to your hospital with a complaint of epigastric and RUQ pain, subjective fever, nausea and vomiting x 3 days. She tells you her twin sister had to have her gallbladder removed after an episode that seemed exactly like the illness she is having.
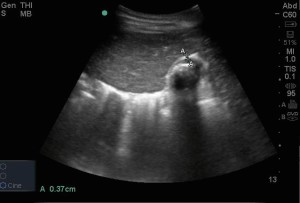
After a brief exam demonstrating mild tenderness in both the epigastric area and RUQ and a possible Murphy’s sign, you put the probe on the patient’s abdomen and see this…
US interpretation?
Case 2: A few weeks later another 45 year old female presents with nearly the same complaint. She has epigastric pain, RUQ pain, nausea and vomiting and weirdly enough, she even looks like your other patient. After an even shorter abdominal exam than you did on the first patient, you again do a bedside sono and see this…
Because you’ve been there, done that, you know the surgery consult will want an “official” sono. You send the patient over to radiology and await the inevitable “critical finding” phone call…
20 minutes later, the phone rings and you are shocked to hear that the critical finding is actually that the patient is s/p cholecystectomy.
So what is the gallbladder looking structure you found on ultrasound??How to tell the difference?
1. Location
GB – within a fossa on the visceral surface of the liver, liver on both sides
Duodenum – medial to the liver, encircling the pancreatic head, liver on only one side
GB – connects in line with the main lobar fissure
Duodenum – no relationship to the main lobar fissure
2. Shape and wall
GB – an encapsulated structure in both longitudinal and transverse views
Duodenum – a true tubular structure, no blind end
GB – an anechoic structure (normal GB) with an ECHOGENIC wall
Duodenum – 5 concentric sonographic layers, like all GI structures, alternating hypo and hyperechoic
3. The Rolling Stone
For a patient with non obstructing gallstones (ie not lodged in the neck)
– Start with the patient in left lateral decubitus position
– Stones will sit in the neck
– Roll the patient so they are left side up
– Stones will slowly roll towards gallbladder fundus
– Debris/air in the duodenum will not move with change in position
4. Peristalsis
– obviously absent in gallbladder
The second RUQ fakeout, once again, demonstrates subtle differences between a non clinically significant variation in gallbladder appearance and a case of significant RUQ pathology.
The above US image demonstrates both walls of the gallbladder around a hypoechoic center. Without measuring, the walls appear thickened and mildly edematous and, in an appropriate clinical setting, would normally be concerning for cholecystitis. Or maybe not? If you actually measured the anterior wall of the gallbladder in this image, it would likely be less than 3mm. Even if it was more than 3 mm, given how contracted the gallbladder is, a slightly larger measurement would likely be a normal variant and not a sign of significant gallbladder disease.
How to tell the difference?
1. MEAUSURE!
- Visually assess if the GB looks contracted
- Get an actual numerical value for the wall, not a visual assessment
2. Look for other signs of cholecystitis
- Stones
- Pericholecystic fluid
- Sono murphy’s sign
Finally, the case of the absent gallbladder which is actually right in front of you.
The image above demonstrates...
How to find this sign?
- Always keep it in mind
- Investigate all shadowing
Hope you enjoyed the first post of 2015!! Happy scanning!
References
- Bortoff GA, Chen MY, Ott DJ, et al. Gallbladder stones: imaging and intervention. Radiographics. May-Jun 2000;20(3):751-66. Bortoff GA, Chen MY, Ott DJ, et al. Gallbladder stones: imaging and intervention. Radiographics. May-Jun 2000;20(3):751-66.
- http://ultrasoundconnection.com/hot-tips-gallbladder-rolling-stones-sign-ultrasound/
andygrock
- Resident Editor In Chief of blog.clinicalmonster.com.
- Co-Founder and Co-Director of the ALiEM AIR Executive Board - Check it out here: http://www.aliem.com/aliem-approved-instructional-resources-air-series/
- Resident at Kings County Hospital
Latest posts by andygrock (see all)
- A Tox Mystery…. - May 26, 2015
- Of Course, US Only for Kidney Stones… - May 18, 2015
- Case of the Month 11: Answer - May 12, 2015
- Too Classic a Question to Be Bored Review - May 5, 2015
- Case of the Month 11: Presentation - May 1, 2015




2 comments for “US vs the RUQ”