Congratulations to this month’s winners. Prizes will go to both dzeccola and edenkim for their excellent answers.
Recap
Oldish gentleman vomiting with epigastric/chest pain, low sat, decreased L side breath sounds, ill appearance. CXR shows a left sided pneumothorax with possibly some rightward mediastinal shift.
Top Three Differential
- Pneumothorax- for sure but is something else going on as well? Boerhaave’s? COPD with bleb rupture? Some kind of trauma we missed?
- MI- could be two things going on
- Still a concern: Pulmonary Embolism! This can present with lower chest, epigastric, or back pain, Our patient is hypoxic, anxious, and borderline tachycardic.
This is a difficult diagnosis but hopefully this write up will help you make a great catch.
“Differentiating esophageal pain from ischemic chest pain can be difficult or impossible in the ED. “(1)
Next Tests or Treatments
- At this point this gentleman is undifferentiated, but we have a high suspicion for some seriously dangerous pathology. Start with the basics: ABC’s +2 large bore IV’s, O2, Monitor, resus bay, IV fluids. Since tension pneumothorax is a big concern, chest tube placement should take place quite quickly.
- ECG, full set of labs including trop and type and cross along with Surgery/GI consults for possible Boerhaave’s.
- Undifferentiated dyspnea always deserves a bedside heart/lung sono.
- Once stabilized, plan for CT chest with PO and IV contrast to better elucidate chest pathology.

As you can see above, his CT chest showed Boerhaave’s injury with a ruptured esophagus and a tension hydropneumothorax! The thoracostomy procedure here could result in a gush of gastric fluid and air, but sometimes the perforation is small – making the findings much more subtle. He needs antibiotics, IV fluids and a trip to the OR with cardiothoracic surgery for a left sided thoracotomy, washout and esophageal repair.
Boerhaave’s Syndrome

Herman Boerhaave
- Rare, population based studies put it at approx. 3/100000 pt years.
- 1/3 cases missed on initial presentation (2)
- The injury is caused by a spontaneous esophageal rupture 2/2 increased esophageal pressure (however, the most common cause of esophageal rupture is now iatrogenic during procedures). The perforation is usually in the distal esophagus on the posterior left side.
- The cause is a sudden, forceful emesis in most cases; however coughing, straining, seizures, and childbirth have been reported as causing perforations as well. Alcohol consumption is associated but unclear if it is causative. (1)
- Subsequent chemical and bacterial mediastinitis and tissue necrosis lead to major sepsis and organ failure. The time between the event, diagnosis, and treatment is critical to minimize the inflammatory response and death from sepsis. Treatment delays of more than 24 hours were associated with a doubling of mortality. Left untreated, mortality approaches 100% (2).
- This disease was first notoriously described by the Dutch physician Herman Boerhaave in 1724. He described the case of Baron Jan von Wassenaer, a Dutch admiral who died of this condition following a gluttonous feast and subsequent regurgitation (4).
Symptoms: (2)
- Pain, vomiting, shortness of breath
- Classically described as acute, severe, unrelenting, and diffuse pain reported in the chest, neck, and abdomen.
- Can radiate to the back and shoulders, or back pain may be the predominant symptom.
- Associated sx: Dysphagia, dyspnea, hematemesis, and cyanosis can be present as well.
- Pain resulting from esophageal perforation is often ascribed to acute myocardial infarction, pulmonary embolus, peptic ulcer disease, aortic catastrophe, or acute abdomen, which can result in critical delays in diagnosis. (1)
Diagnosis (3)
- Chest xray will show effusion, pneumothorax, or pneumomediastinum in 90% of cases
- CT of the chest/abdomen with oral and IV contrast is usually diagnostic
- findings include pneumomediastinum, contrast leak, pneumothorax, pleural effusion
- Can consider endoscopy for equivocal case diagnosis and for management.
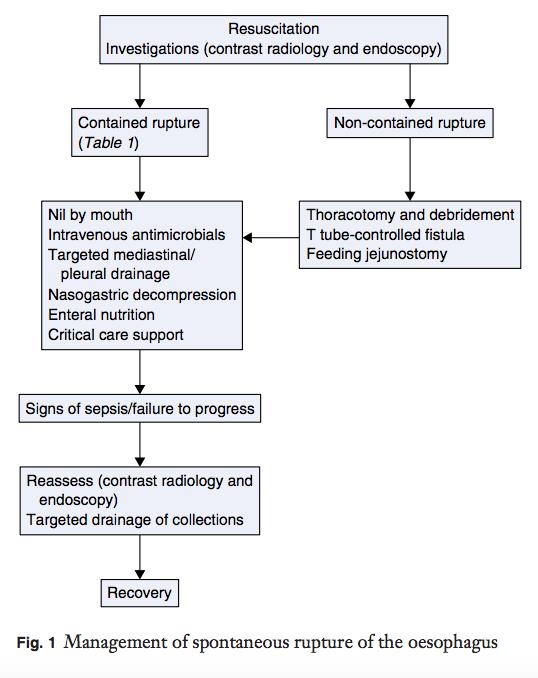
Treatment (3)
- ABC’s/ resuscitation
- NPO
- NG tube
- You should probably do this in conjunction with CT Surgery
- Antibiotics
- Chest tube if pneumothorax present
- Usually OR vs IR for thorax/mediastinal drainage
- Some cases now can be managed conservatively or with delayed drainage
- Often will require Critical Care
- +/- endoscopy for diagnosis or therapy
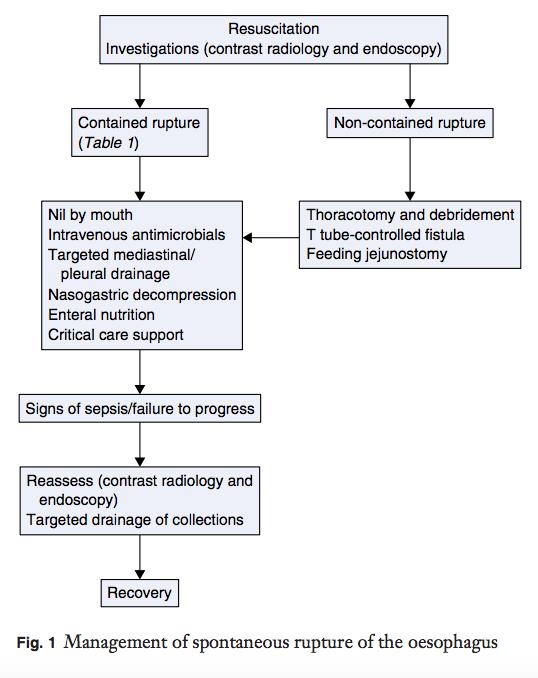
(figure from source 2)
By Dr. Carl Alsup and Dr. Andrew Grock
- Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 7e. Chapter 80. Esophageal Emergencies, Gastroesophageal Reflux Disease, and Swallowed Foreign Bodies
- Blencowe, et al. Spontaneous oesophageal rupture. BMJ 2013;346:f3095
- Griffin, et al. Spontaneous rupture of the oesophagus. British Journal of Surgery 2008; 95: 1115–1120
- Lugduni Batavorum Boutesteniana 1724
The views expressed on this blog are the author's own and do not reflect the views of their employer. Please read our full disclaimer
here. Any references to clinical cases refer to patients treated at a virtual hospital,
Janus General Hospital.
The following two tabs change content below.