It’s a slow Sunday afternoon in the mythical ED that all of our blog posters seem to work in and you see a 70 year old male with a history of HTN, HLD and renal stones. He is mildly hypertensive and reports sharp flank, occasional abdominal pain and hematuria. These symptoms, he tells you, feel “just like kidney stones.” Other than the fact that his abdominal exam is limited by obesity, his exam is unremarkable.
You send a UA, a shock panel to check the patient’s creatinine, give the patient analgesia and of course, plan to do a bedside ultrasound.
30 minutes later the patient’s pain has resolved, his creatinine is normal, he’s got some RBCs in his urine and he’s ready to walk out the door, promising to see his urologist the next morning….
Remembering a September 2014 NEJM multicenter study, you opt to not CT scan this patient. Right? Remember, 2759 patients were randomized to either ED US, radiology US or CT scan. None of the patients went on to have complications directly related to their study selection and there was a comparable amount of “missed” diagnoses in each group. The study also reports statistically significant decreases in radiation between the US and CT groups, even when CTs ordered after US were accounted for.
Welcome to the choose your own adventure portion of this blog post, inspired by my recent oral board exam…
Would you:
A: Let the patient go without an ultrasound, he seems fine and has good follow up
B: Do a renal sono and let the patient go if its normal
C: Do a renal sono and let the patient go if it shows signs of mild hydro
Either way, the patient goes home and comes back the next day…
During a crazy Monday afternoon in the same mythical ED and your patient rolls in by EMS. He ‘s reporting increasing pain, now more in the abdomen, and EMS tells you he’s relatively hypotensive with a systolic BP of 100. His exam is basically unchanged from the day before.
You’re baffled and exclaim…
“He felt great, I didn’t even need to do a sono.”
OR
“His ultrasound was normal, not a speck of hydro”
OR
“His ultrasound was fine, only mild hydro”
But what about the aorta…
The idea that an AAA must be kept on the differential for anyone with flank pain is not a new one. In fact, its something I remember learning way back in my EM clerkship. However, the fact that renal colic is so much more common that a symptomatic AAA and the push to decrease the amount of CT scans we do to identify recurrent kidney stones, can often lead to a situation where AAAs are missed. We scan lots of kidneys for hydro, but do we scan all of those patients for AAA??
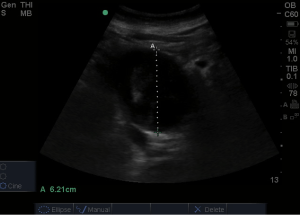
This patient’s ultrasound may have demonstrated this:
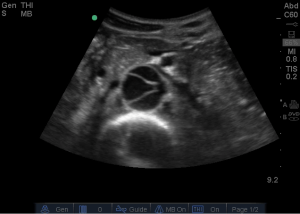
or even this
These images show (A) a AAA with thrombus and (B) an aortic dissection with dissection into the renal artery.
Both of these entities are known to cause abdominal and flank pain and are more common in older patients with multiple co-morbidities but their presentations can often closely mimic that of renal colic.
One study of 134 patients with AAA reported these statistics:
- Eighteen percent had an initial misdiagnosis of nephrolithiasis
- All were older than 60 years
- Eighty percent had a pulsatile mass noted by at least one examiner
- Forty-three percent had hematuria on urinalysis
- Delay of diagnosis of AAA in the ED was associated with higher mortality and morbidity rates than in the group who received the correct diagnosis promptly
- – all patients with delay in diagnosis greater than 5 hours died
Keep in mind, the NEJM study described above seemed both convincing and overwhelming, it’s important to realize that this study excluded patients whose physicians included AAA on their differential diagnosis. This study also focused only on the use of US as the first test – not necessarily the only test the patient needs.
So what do we do about this? Obviously, we do MORE ULTRASOUND! Its not enough to consider AAA on your differential, you have to rule it out. Be sure you scan the aorta when you’re worried enough to scan the kidney, otherwise…urine trouble.
By Michelle DiMare
References
Borrero E, Queral LA. Symptomatic abdominal aortic aneurysm misdiagnosed as nephroureterolithiasis. Ann Vasc Surg. Apr 1988;2(2):145-9.
Smith-Bindman R, Aubin C, Bailitz J, et al. Ultrasonography versus Computed Tomography for Suspected Nephrolithiasis. N Engl J Med. 2014;371(12):1100–1110.
andygrock
- Resident Editor In Chief of blog.clinicalmonster.com.
- Co-Founder and Co-Director of the ALiEM AIR Executive Board - Check it out here: http://www.aliem.com/aliem-approved-instructional-resources-air-series/
- Resident at Kings County Hospital
Latest posts by andygrock (see all)
- A Tox Mystery…. - May 26, 2015
- Of Course, US Only for Kidney Stones… - May 18, 2015
- Case of the Month 11: Answer - May 12, 2015
- Too Classic a Question to Be Bored Review - May 5, 2015
- Case of the Month 11: Presentation - May 1, 2015

4 comments for “Of Course, US Only for Kidney Stones…”