By Baruch Berzon MD and Richard Sinert MD
Case Presentation
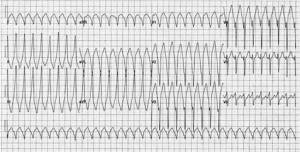
A 32 year-old male presents in August to EMS with complaints of “flutter in my chest” and light-headedness for an hour. The paramedics find a young man in mild distress who is Diaphoretic with a heart rate of 220 and a blood pressure of 110/69. The 3-lead ECG shows a wide-complex tachycardia at a rate of 220 BPM. They obtain IV access and preform a 12 –lead. They transmit the 12-lead and call you for consultation:
(From the European Society of Cardiology)
Clinical questions
- Interpret the 12 lead?
- Should they attempt to treat this chemically or electrically? If chemically, what is the drug of choice?
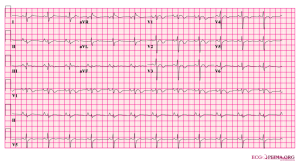
- They converted the patient and get the following repeat ECG:
- Now the patient is in your ED, his vital signs are normal. In addition to routine lab testing and cardiologic consultation for Ventricular Tacycardia, what else would you do for the care of this patient?
Overview with learning points
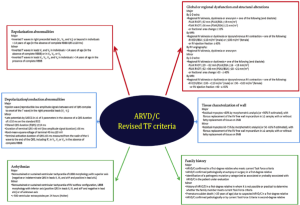
Arrhythmogenic Right Ventricular Dysplasia/Cardiomyopathy or ARVD/C is one of the most arrhythmogenic forms of inherited cardiomyopathy and a cause of sudden cardiac death (SCD) in the young.1 ARVD is the most common cause of sudden cardiac death in young athletes after Hypertrophic Cardiac Myopathy. 4
Pathophysiology-(Journal of Cariology)
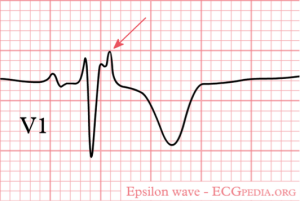
The classic ECG finding is an Epsilon wave which is a low amplitude signal at the end of the QRS in V1-V3.
One can infer from the above that the testing required to make a definite diagnosis are not readily available in the ED. However a history of SCD in the family, previous unexplained syncopal episodes and an ECG with characteristic findings should raise the clinical suspicion for ARVD/C and prompt further testing.
Long term treatment includes antiarrhythmic drugs for prevention of arrhythmias and implantation of an AICD. Catheter ablation with new 3D mapping has heterogeneous results with success ranging from 45-85%. In patients with extensive heart failure or drug-refractory VT’s, heart transplantation is the last resort but this occurs very rarely.
In summary…
ARVD/C is a heterogenic disease that presents in young patients with syncope, VT’s or sudden cardiac death. The epsilon wave might be the first clue for the emergency physician to the possibility of ARVD/C and should prompt a through history, exam and appropriate diagnostic testing.
Extra! Extra! Read all about it–
Did you know that some ARVD/C had involvement of predominantly the LV? It should be called ALVD/C 🙂 ?
Did you know that sometimes ARVD/C is recessive and involves a cutaneous phenotype? (eg. Naxos disease or Carvajal syndrome)
That there is a known link between ARVD/C and myocarditis that is still waiting for YOU to clearly define?
FOAMED and REFERENCES:
http://journal.frontiersin.org/article/10.3389/fphys.2012.00023/full comparison to RVOT
http://www.heartpearls.com/tag/epsilon-wave
http://lifeinthefastlane.com/ecg-library/basics/epsilon-wave/
http://www.af-ablation.org/?page_id=2034
http://www.revespcardiol.org/en/arrhythmia-and-right-heart-disease/articulo/13154581/ RVOT and Brugada looks at as well
- Arrhythmogenic right ventricular dysplasia/cardiomyopathy: Clinical challenges in a changing disease spectrum. te Riele A. et al; Trends in Cardiovascular Medicine, Volume 25, Issue 3, April 2015, Pages 191–198
- Cardiovascular causes of sudden death in young individuals including athletes. Basso C. et al; Cardiology Review, 7 (1999), pp. 127–135
- Population-prevalent desmosomal mutations predisposing to arrhythmogenic right ventricular cardiomyopathy. Lahtinen AM et al; Heart Rhythm.2011 Aug;8(8):1214-21
- Impact of new task force criteria in the diagnosis of arrhythmogenic right ventricular cardiomyopathy. Giuseppe F. et al; International Journal of Cardiology 171 (2014) 179–183
- Current and state of the art on the electrophysiologic characteristics and catheter ablation of arrhythmogenic right ventricular dysplasia/cardiomyopathy. Chung F-P, et al; J Cardiol (2015),
jshibata
- Resident Editor-in-chief of blog.clinicalmonster.com
- Blog author of kchemimage.wordpress.com/category/clinical-radiographs/
- Co-author of the Resident Journal Review for AAEM’s Common Sense newsletter.
- EM/IM Resident at Kings County Hospital
Latest posts by jshibata (see all)
- Tox Craze - July 30, 2015
- PE or not PE, that is the question… - July 29, 2015
- Right on Target: A Petite Peds Post - July 6, 2015
- ARVD/C - June 18, 2015
- A dose of primary care for hyperglycemia in the ED: optimizing the discharge. - May 5, 2015

1 comment for “ARVD/C”