The EKG is an integral diagnostic tool in EM let alone the whole of medicine. It is a rapid, reliable and cost-effective method to aid in the diagnosis of cardiac pathology including ischemic and arrhythmic events. So how did it come about?
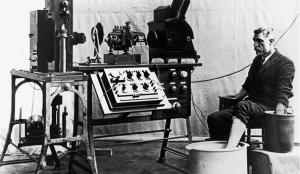
The 12 lead EKG was innovated via multiple innovations over two centuries. Dr. Luigi Giovanni was the first to point out electrical activity in animal tissue in 1786 in Italy. Heart electrical activity was demonstrated in frogs in the 19th century. In 1877, Augustus Waller demonstrated the first electrocardiogram (although the term was not penned until after) using a capillary electrometer and electrodes, relating electrical activity to ventricular contraction.
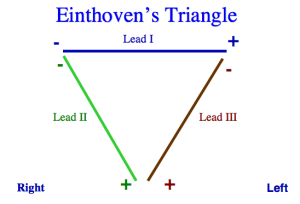
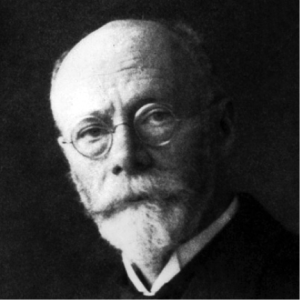
It was Dr. Willem Einthoven from the Netherlands who innovated the EKG for clinical use by refining the electrometer and delineating PQRST waves. He used three limb leads, which became known as Einthoven’s triangle. Einthoven received the Nobel Prize in physiology and medicine for his work in creating the first iteration of the clinical EKG and foundation for future innovations to come.
The EKG made its clinical debut in the US at Mt. Sinai hospital in 1909. EKGs were initially used to study arrhythmias, with atrial fibrillation being described in 1909. By 1930, the EKG was recognized as being an important tool in differentiating cardiac from non-cardiac chest pain, with some EKG patterns of ischemia recognized as pathognomonic for MI.
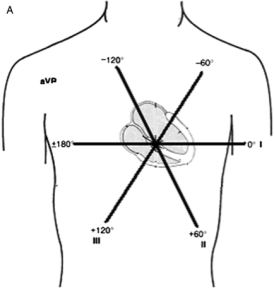
However, it was evident that many MIs were missed on routine three lead EKGs, and that ‘silent areas’ of the heart’s electrical activity were not detectable. In 1934, Dr. Frank N. Wilson of the University of Michigan (my alma mater!) developed the concept of the ‘central terminal,’ or reference terminal by combining the limb electrodes. A galvanometer measured the potential difference between a single electrode from the body surface and this ground or ‘central terminal.’ The potential difference between that point on the body and the central terminal where there was zero potential (ground terminal) created a ‘unipolar lead.’ In comparison the initial limb leads developed by Einthoven could be thought of as ‘bipolar’ leads since they measured the potential difference between two sites with nonzero potentials. Wilson’s unipolar leads were placed in a horizontal plane, creating V1-V6, with ‘V’ standing for vector. These became known as the precordial leads and would revolutionize the detection of ischemic heart disease on EKG.
In 1942, Dr. Emanuel Goldberger in New York added three unipolar frontal leads using Wilson’s central terminal and three limbs, creating aVL, aVF and aVR, in effect reducing the frontal degree increments to 30 degrees and allowing an even higher detailed EKG. These leads required augmentation to match the rest of the leads, explaining the small ‘a’ in the lead names. This was also the first time a positive electrode was placed over the right arm, against the direction of the electrical activation, leading to the strange looking a-VR with negative polarity on EKG. The invention of the unipolar limb leads concluded the major advancement toward the 12-lead electrocardiogram which we use to this day, especially in the Emergency Department!
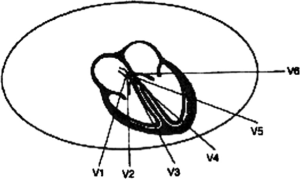
Frank Wilson’s unipolar precordial leads allowed for a horizontal plane of detection and increased sensitivity for ischemic events

The combination of unipolar and bipolar limb leads allowed for higher detailed EKGs along the frontal plane
AlGhatrif, Majd, and Joseph Lindsay. “A brief review: history to understand fundamentals of electrocardiography.” Journal of community hospital internal medicine perspectives 2.1 (2012).
nisasi
Latest posts by nisasi (see all)
- Legends of Medicine – History of the EKG - July 16, 2015