Written by Randi Ozaki
…and probably one of the more annoying clinical questions that we’re faced with in the ED. PERC (pulmonary embolism rule-out criteria), D-dimer and Well’s criteria have been discussed ad nauseam, but the question I pose to you, is how does ultrasound fit in to our algorithm and can it help aid us in our diagnosis and/or management in patients suspected of having a PE?
CT PA is the diagnostic modality of choice in patients suspected of having a PE, however there are many instances where CT may not be possible or even feasible. The fact that patients require a good IV placed in the antecubital fossa is often a rate-limiting step and in a busy ED, it may be some time before a line is successfully placed. Patients with renal insufficiency are unable to receive contrast and in pregnant patients, the risk of radiation exposure to the fetus often precludes the possibility of a CT scan. Additionally, radiation exposure to young reproductive age patients in general is something optimally avoided. Furthermore, patients with massive PE may be too unstable to leave the ED to obtain a CT scan.
Rock. Me. Hard Place.
There is a solution: ultrasound, of course!
While direct visualization of a thrombus in the right atrium or pulmonary artery is possible, it is a rare finding. There are, however, indirect findings on ultrasound which may heighten or confirm your suspicion of PE.
Echocardiography and evaluation of right ventricular strain or dysfunction may heighten one’s suspicion of a clinically significant PE. Patients with unexplained hypotension or shock, secondary to PE will show signs of RV dysfunction. The absence of such findings on echo, should lead the provider to seek an alternative explanation for the patient’s instability. Unfortunately, in patients without shock or hypotension and who have a normal echo, the diagnosis of pulmonary embolism cannot be ruled out.
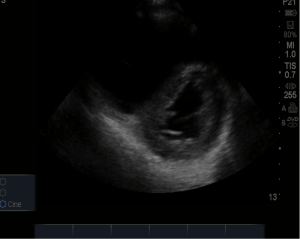
What do you see in the ultrasound below?
Answer:
What is McConnell’s sign?
Answer:
Look for it in the apical four-chamber view. This finding is 94% specific for RV dysfunction secondary to PE, however only has a 77% sensitivity. There are other causes of RV dysfunction (pulmonary hypertension etc.), however these tend to cause more global hypokinesis of the RV.
What are other indirect indicators of a possible PE?
Answer:- IVC dilatation without inspiratory collapse
- DVT on lower extremity ultrasound.
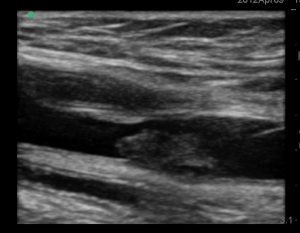
This is an example of a lower extremity DVT seen in the longitudinal plane.
Compressive venous ultrasonography to evaluate for DVT is another useful diagnostic tool that can be used in patients with a suspected PE. It is readily available and non-irradiating. Diagnosis of a proximal DVT has a high positive predictive value for PE, and would allow for initiation of anticoagulant therapy without the need to wait for CT results. However, as with echo, a negative DVT study does not exclude the diagnosis of PE.
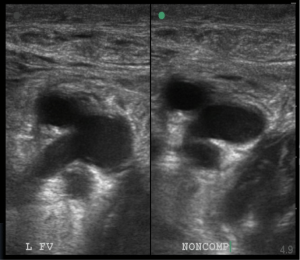
The right panel shows no collapse of the femoral vein during compression.
Summary:
1. Aside from direct visualization of a thrombus, there is no direct way of diagnosing PE on ultrasound.
2. A negative echo and negative DVT does not exclude the diagnosis of PE.
3. The ability to find a DVT on exam or signs of RV strain in patients suspected of PE will allow for faster initiation of appropriate therapies.
4. Look for other causes of hypotension in patients without signs of RV strain on bedside echo
References:
Borloz et al. “Emergency department focused bedside echocardiography in massive pulmonary embolism.” The Journal of Emergency Medicine. 41(6): 658-660, 2011.
Squizzato et al. “ “Point-of-care ultrasound in the diagnosis of pulmonary embolism.” Crticial Ultrasound Journal. 7:7, 2015.
jshibata
- Resident Editor-in-chief of blog.clinicalmonster.com
- Blog author of kchemimage.wordpress.com/category/clinical-radiographs/
- Co-author of the Resident Journal Review for AAEM’s Common Sense newsletter.
- EM/IM Resident at Kings County Hospital
Latest posts by jshibata (see all)
- Tox Craze - July 30, 2015
- PE or not PE, that is the question… - July 29, 2015
- Right on Target: A Petite Peds Post - July 6, 2015
- ARVD/C - June 18, 2015
- A dose of primary care for hyperglycemia in the ED: optimizing the discharge. - May 5, 2015