Written by Alex Brevil
A 52 y/o woman w/ fibromyalgia is found alone in her room in a confused state by her maid. She recently lost all of her retirement money and constantly “Blames Obama.” She is then rushed to the emergency room where she is found to be disoriented x2 (oriented to the president only) w/ flushed skin. The patient begins to seize just after the nurse takes her vitals (and the med student faints).
VS- pulse- 130bpm, BP- 95/60, RR- 24, T-101.5
PE- Pupils 6mm b/l, distended lower abdomen, absent bowel sounds
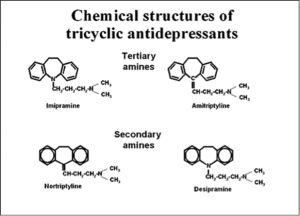
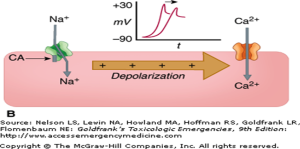
What is the most likely diagnosis? TCA (or TC-Eh? in Canadian) toxicity!! Common Drugs– Amitriptyline, Imipramine. Clomipramine, Nortriptyline Indications– Depression, panic disorder, obsessive compulsive disorder, chronic pain syndromes (fibromyalgia, neuropathic pain, migraine ppx) TOXICITY….. TREATMENT ABC’s first… Then… What about Physostigmine (Cholinesterase Inhibitor)? Remember CO = HR x SV (Alpha antagonist effects cause low bp and HR is keeping up the cardiac output, therefore, slowing this down with a cholinergic drug theoretically can cause a dangerous drop in cardiac output!!!!! Summary 1. Take a good medical history and physical exam 2. Early intervention (ABC’s, EKG!!!!!) 3. Early correction of conduction abnormalities w/ Sodium Bicarb. 4. No physostigmine… References: Lynch R. Tricyclic antidepressant overdose. Emerg Med J 2002; 19:596 Kerr GW, McGuffie AC, Wilkie S. Tricyclic antidepressant overdose: a review. Emerg Med J 2001; 18:236. Liebelt, EL, Francis, PD. Chapter 57: Cyclic Antidepressants. In Goldfrank LR et al [eds], Goldfrank’s Toxicologic Emergencies (7th Edition). New York, McGraw-Hill, 2002. Tran TP, Panacek EA, Rhee KJ, Foulke GE. Response to dopamine vs norepinephrine in tricyclic antidepressant-induced hypotension. Acad Emerg Med 1997; 4:864 Pentel P, Peterson CD. Asystole complicating physostigmine treatment of tricyclic antidepressant overdose. Ann Emerg Med 1980; 9:588. Mills KC. Chapter 171. Cyclic Antidepressants. In: Tintinalli JE, Stapczynski J, Ma O, Cline DM, Cydulka RK, Meckler GD, T. eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 7e. New York, NY: McGraw-Hill; 2011
 Mad as a Hatter (CNS symptoms)
Mad as a Hatter (CNS symptoms) Dry as a Bone (urinary retention, decreased bowel sounds, dry mucous membranes).
Dry as a Bone (urinary retention, decreased bowel sounds, dry mucous membranes).
jshibata
Latest posts by jshibata (see all)