Hey everyone. It’s time for another peds blog. We were in a short hiatus but now we are back on. I figured that while we were in our procedure blog, we should cover a topic involving the little ones. And in this blog, I actually mean the little ones (<12 years). Picture the scenario where you have a child in front of you in the resuscitation bay and he cannot protect his airway. You look into the mouth and all you see is tongue and secretions. This child is having an anaphylactic reaction to peanuts and has severe angioedema, anesthesia is nowhere to be found and you have seconds until this child goes into cardiac arrest. What do you do?
What about the trauma victim that has such extensive facial injuries that performing endotracheal intubation may actually harm the patient and they need an emergent airway in the ED? How do you secure that airway?
This month we will be talking about the surgical airway in a child, and I mean less than 12 years of age. Percutaneous transtracheal jet ventilation (PTJV) is the preferred surgical airway for children under 12 because of the small tracheal diameter and the larynx is more rostral with a more prominent hyoid bone on which an open cricothyrotomy is often impossible. Some reports have recommended PTJV only as a transient resuscitative measure for emergent situations in which endotracheal intubation or other ventilation methods are not feasible. PTJV is widely thought of as a temporizing procedure to be maintained for only 30 minutes at best. However, animal experiments and clinical studies have demonstrated that transtracheal ventilation is an effective, quick, fairly simple, and safe way to obtain and maintain an airway for a prolonged period of time.
In a life-threatening situation in which tracheal intubation and bag-mask-valve ventilation cannot be performed to restore adequate gas exchange during acute respiratory failure, PTJV must be entertained as a viable interim maneuver. Under such circumstances, PTJV with a large bore needle provides immediate oxygenation and ventilation by providing adequate gas exchange and ensuring the patency of the airway until a definitive procedure such as oral intubation with bronchoscopy followed by surgical tracheostomy can be performed. Transtracheal jet ventilation may be used even with partial airway obstruction.PTJV can force oropharyngeal secretions out of the proximal trachea and may force a foreign body out of the proximal trachea (in cases of partial airway obstruction). However, upper airway patency is required for exhalation during PTJV,
Indications
- Indications for percutaneous transtracheal jet ventilation (PTJV) are similar to those for surgical cricothyrotomy.
- PTJV is indicated in any situation in which intubation is contraindicated or cannot be achieved.
Absolute Contraindicatons
- If a definitive airway can easily and rapidly be secured with endotracheal intubation, percutaneous transtracheal jet ventilation (PTJV) is not used.
- PTJV is not used in the presence of known significant direct damage to the cricoid cartilage or larynx.
Relative Contraindications
- PTJV can be used in the presence of partial airway obstruction provided that appropriate-sized catheters are used.
- Airway obstruction below the vocal cords that renders exhalation difficult or impossible is a relative contraindication.
Equipment
- Lidocaine 1-2% at a dose of 2-3 mL is generally sufficient for local skin anesthesia via infiltrative administration in patients who are alert and awake. Injection of a small amount of anesthetic percutaneously into the trachea itself will blunt the cough response as well.
- Oxygen source with a flow at 10-15 L/min
- Commercial bag-valve-mask device (Ambu bag) that includes noncollapsible oxygen tubing and a reservoir bag
- Large-bore, over-the-needle intravenous catheter (14 ga)
- Plastic syringe, 3 mL, with Luer lock tip, that fits tightly into a 7.5-mm inner diameter endotracheal tube adapter
- Inner adapter of 7.5 mm endotracheal tube
Equipment assembly
- Connect the intravenous catheter to a 3-mL syringe barrel (with its plunger removed).
- Connect the 3-mL syringe barrel to a 7.5-mm inner diameter endotracheal tube adapter.
- Lock the valve of the bag-valve-mask device and connect its oxygen tubing to an oxygen source with a flow at 10-15 L/min.
- Connect the endotracheal tube adapter to the bag-valve-mask device.
- Manually ventilate
- Recommended Inspiration:Expiration ratios
– Standard – 1:4 to 1:5
– Supraglottic airway obstruction – 1:9
(need more time to let gas escape, otherwise may build up too much pressure in the lungs)
Positioning is the same as when performing a cricothyroidotomy.
Needle cricothyroidotomy
- Needle cricothyroidotomy should be performed with universal precautions and sterile technique. The puncture site is cleansed with povidone-iodine solution after sterile gloves have been donned.
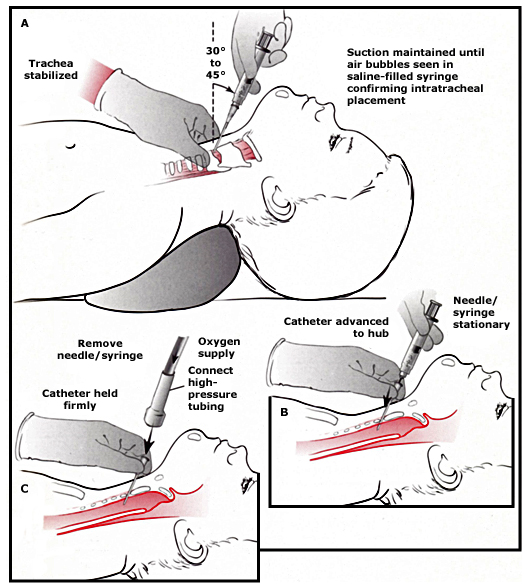
- Hold the trachea in place and provide skin tension with the thumb and middle finger of the non-dominant hand placed on either side of the trachea. Use the index finger to palpate the cricothyroid membrane.
- Hold a 3 to 10 mL syringe half-filled with saline attached to the needle or the over-the-needle IV catheter in the dominant hand.
- Place the needle in the midline of the neck at the inferior margin of the cricothyroid membrane (to avoid the cricothyroid blood vessels located superiorly and laterally). Direct it caudally (toward the feet) at an angle of 30 to 45 degrees.
- Puncture the skin and subcutaneous tissue. Advance the needle while continuously applying negative pressure on the syringe, until air bubbles are seen, confirming intratracheal placement.
- Advance the catheter forward off the needle until its hub rests at the skin surface. Remove the syringe and the needle.
- A small nick in the skin may be needed to facilitate passage through the dermis into the subcutaneous tissue. Thin catheters may kink or bend in the presence of too much resistance during insertion.
- Reattach the syringe to the catheter and again aspirate for air to confirm that the catheter remains in the trachea.
- Hold the catheter firmly in place at all times or delegate an assistant to do this to reduce the chance of kinking or dislodgement, even after it has been secured with suture material
Performing transtracheal ventilation
- Connect the catheter to high pressure tubing (connected to a valve and a source of 100 percent oxygen) or to a bag-valve-mask (Give a few ventilations to reconfirm placement and ensure that the equipment is functioning properly.
- Fix the catheter in place with a suture or a tracheostomy tie, as possible.
- Interpose a capnometer in the circuit to monitor end tidal CO2, if possible.
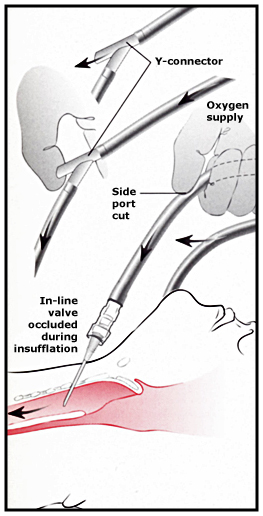
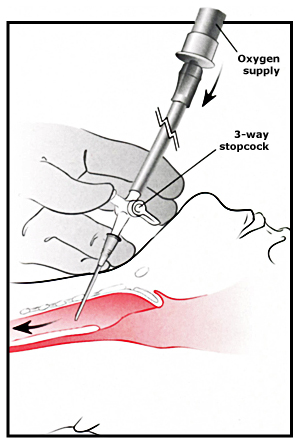
- Begin regular by intermittently occluding the side port, y-connector, or stopcock or by ventilations with the self-inflating resuscitation bag, depending on the system in use.
- Use I:E ratio of 1:4 to 1:5, with a breath rate of 10 to 12/min for most children. With partial or complete upper airway obstruction, use the ratio of 1:8 to 1:10 with a breath rate of 5 to 6/min to reduce the risk of pulmonary barotrauma. Adjust these ratios based on clinical monitoring, blood gas measurements, and chest radiography.
- Stand clear and observe universal precautions as oropharyngeal secretions may sometimes be expelled through the patient’s mouth and nose with great force.
Complications
- Complications with this technique include aspiration, bleeding, pneumothorax, subcutaneous emphysema, barotrauma (eg, pneumothorax, pneumomediastinum), catheter-related problems (eg, obstruction or blockage of the catheter, kinking of the catheter, catheter displacement, misplaced or unsuccessful needle or catheter placement), and inadequate ventilation.
- The exact incidence of complications with percutaneous transtracheal jet ventilation (PTJV) is not known, but it is thought to be low, considering that the complication rate of translaryngeal puncture alone is in the range of 0.03-0.8%.
- Disadvantages of PTJV include the following:
– Incomplete control of the airway with subsequent greater potential for aspiration than with a cuffed endotracheal tube.
– Potential for barotrauma (subcutaneous emphysema or pneumothorax) if exhalation is inadequate and airway pressure is elevated
References
– Arch Otolaryngology Head Neck Surg. 2005;131:886-890 Percutaneous Transtracheal Jet Ventilation in Head and Neck Surgery Yusuf Gulleth, BA; Jeffrey Spiro, MD
– Jorden RC. Percutaneous transtracheal ventilation. Emerg Med Clin North Am. Nov 1988;6(4):745-52.
– Manoach, Paladino, Sinert et al. Percutaneous transcricoid jet ventilation compared with surgical cricothyroidotomy in a sheep airway salvage model.
– Medscape: Percutaneous Transtracheal Jet Ventilation
– Patel, RG, Norman, JR The technique of transtracheal ventilation. J Crit Illness 1996; 11, 803-808
– Patel, RG Percutaneous Transtracheal Jet Ventilation: A Safe, Quick, andTemporary Way To Provide Oxygenation and Ventilation When Conventional Methods Are Unsuccessful
– Stothert JC Jr, Stout MJ, Lewis LM, Keltner RM Jr. High pressure percutaneous transtracheal ventilation: the use of large gauge intravenous-type catheters in the totally obstructed airway. Am J Emerg Med. May 1990;8(3):184-9.
– Walls RM. Management of the difficult airway in the trauma patient. Emerg Med Clin North Am. Feb 1998;16(1):45-61.
– UpToDate: Needle cricothyroidotomy with Percutaneous Jet Ventilation
Smelendez
Latest posts by Smelendez (see all)
- Peds In A Pod: My Child Fell & Hit His Head, HELP! - March 18, 2013
- Peds In A Pod: Percutaneous Transtracheal Jet Ventilation - December 3, 2012
- Peds in a Pod: C-spine Clearance - July 31, 2012
- Peds in a Pod: So What’s the Deal With Bronchiolitis? - June 10, 2012
- Peds in a Pod: Submersion - May 11, 2012