This is a fictitious patient seen at a fictitious hospital called Janus General. Don’t believe me? I’m on staff there – see
After seeing your 44th URI of the day in the Peds ER, you get a call on the batphone – a 4 year old female, altered mental status, eta 4 minutes. You prep the resus room and assign roles.
On arrival, the patient begins to have a tonic-clonic seizure. Per broselow tape, you give the correct dose of IM midazolam with resolution of the seizure.
CC: AMS now with generalized tonic-clonic seizure
HPI: 4 year old female, no past medical history was found on bathroom floor. The medicine cabinet was open with pill bottles scattered on ground, many open. Mom and Dad together take medication for HTN, DM, and CHF but do not know the medications’ names. Sister takes allergy medicine, sleeping medicine, and OCPs. The cabinet has the usual over-the-counter medications (motrin or tylenol or both, itching medicine pills, neosporin, vitamins) as well.
ROS fully negative prior to being found down.
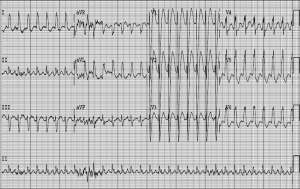
VS HR 180 (and appears WIDE!), RR 15, BP 140/70, Rectal Temp 98.5, O2stat 100% on NRB.
PE: Child is responsive to touch, groans, PERRL, moves all 4 extremities, warm skin, dry MM, +gag, heart/lung/abdomen exam unremarkable.
EKG
1. Please provide a thorough differential including leading diagnosis.
2. Please provide a brief summary of appropriate management for your top diagnosis and/or for the patient.
By Dr. Andrew Grock
Special thanks to Dr. Khadpe for his invaluable feedback on the Case of the Month episodes #1 and #2.
andygrock
- Resident Editor In Chief of blog.clinicalmonster.com.
- Co-Founder and Co-Director of the ALiEM AIR Executive Board - Check it out here: http://www.aliem.com/aliem-approved-instructional-resources-air-series/
- Resident at Kings County Hospital
Latest posts by andygrock (see all)
- A Tox Mystery…. - May 26, 2015
- Of Course, US Only for Kidney Stones… - May 18, 2015
- Case of the Month 11: Answer - May 12, 2015
- Too Classic a Question to Be Bored Review - May 5, 2015
- Case of the Month 11: Presentation - May 1, 2015

3 comments for “Case of the Month #2-Presentation, 8/1/14”