Thanks to Dr. Freedman for today’s Morning Report!
Digoxin Toxicity
Background:
- Naturally occurring chemical compounds
- Na+/ATPase Channel blockers
- Prone to poisoning
- Large volume of distribution
- Long half-life, ~36 hours
- Narrow therapeutic window, 0.6 – 1.3 ng/mL
Digoxin:
- An Old Drug: CHF, A fib
- ~2% of all international patients.
- One of the 50 most commonly prescribed in U.S.
- 1,601 acute ingestions in U.S. in 2011
- In U.S., 1% of outpatients and ~18% of NH patients will develop toxicity
- 0.4% of all U.S hospital admissions
Plant Cardiac Glycosides:
- Many different flowering plants
- Foxglove, oleander, lily of the valley et al.
- 2.6% of all toxic plant exposures
- 1,336 in U.S. in 2011
Acute Ingestions
Epidemiology: the young (one pill kill)
- Adults: LD50 10mg
- Pediatrics: LD 50 0.3mgkg
Presentation: Cardiac symptoms
- Bradycardia +/- hypotension
- Dysrhythmias
- Sinus
- Junctional
- AV block
- Slow a fib/flutter
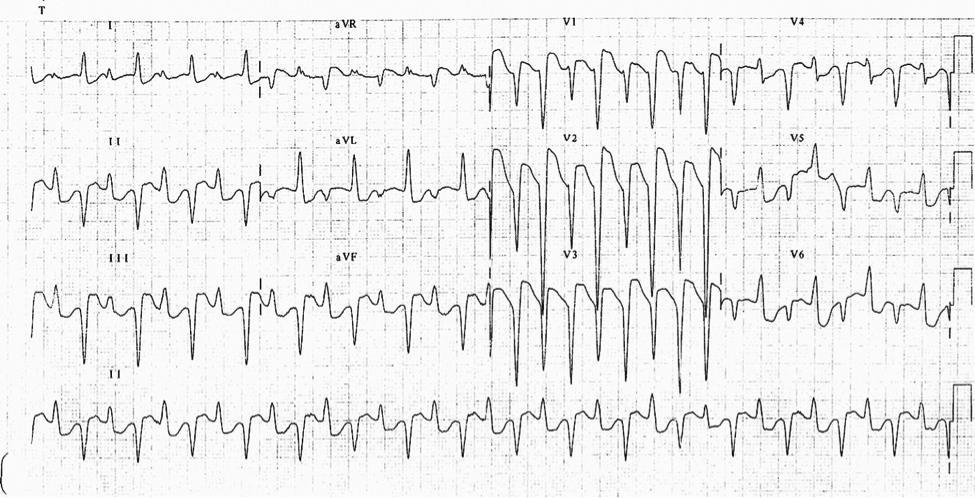
- Bidirectional V tach
Chronic Toxicity
Epidemiology: Elderly, chronically ill
- Normal or sub-therapeutic levels
- Triggered by:
- Electrolyte disturbance
- Hypovolemia
- Drug-drug interactions
Presentation: Often non-specific
- Altered mental status, weakness, fatigue
- Nausea/vomiting, abdominal pain
- Visual complaints
ECG findings:
- “Scooped” ST segment, Digitalis Effect
- Any of the acute dysrhythmias
ED Management
- ABCs
- Supportive care
- Correction of electrolyte disturbance
- H+P
- Acute?
- When, how much?
- Acute?
- Chronic?
- Index of suspicion
- Trigger?
- Lab Studies
- Digoxin Level
- 6 hour level
- Earlier levels don’t reflect steady state
- Potassium
- Marker of acute toxicity
- Prognostic value
- Digoxin Level
- Interventions
- Bowel decontamination
- Consider if <1-2 hours
- Atropine
- Not contra-indicated….
- Pacing
- Not recommended
- Dialysis
- Not plausible
- Digi-Fab
- Ingestion of 10 mg in adults, or 0.3 mg/kg in children
- Acute ingestion with steady-state level > 10ng/mL
- Chronic ingestion with steady-state level > 6ng/mL
- Any dysrhythmia, irrespective of level
- Serum potassium > 5.5 in acute ingestion
- Any plant toxicity
- Bowel decontamination
Emergency Medicine Mythology:
Intravenous calcium is contraindicated in digoxin toxicity. “Stone Heart” Syndrome. Based on case studies. No data to support theory. Weak data exist to suggest calcium is safe in dig-toxic. Bottom-line: Give IV calcium if you suspect hyperkalemia.
Bidirectional V tach
The views expressed on this blog are the author's own and do not reflect the views of their employer. Please read our full disclaimer here. Any references to clinical cases refer to patients treated at a virtual hospital, Janus General Hospital.
The following two tabs change content below.


Jay Khadpe MD
Editor in Chief of "The Original Kings of County"
Assistant Professor of Emergency Medicine
Assistant Residency Director
SUNY Downstate / Kings County Hospital
Latest posts by Jay Khadpe MD (see all)
- Morning Report: 7/30/2015 - July 30, 2015
- Morning Report: 7/28/2015 - July 28, 2015
- IN THE STRETCHER INSTEAD OF BESIDE IT - July 22, 2015
- Morning Report: 7/14/2015 - July 14, 2015
- Morning Report: 7/10/2015 - July 10, 2015
