Today’s Morning Report is courtesy of Dr. Melendez (presented 4/12/2012). Follow the along and think about how you would handle this scary presentation.
A mother brings her 9 day old infant in because “she has not urinated in the past 12 hours and she is very sleepy”. VS: BP70/30, HR 86, RR 35, Trectal: 98.7, O2 sat 100%RA. On PE the baby appears lethargic, has sunken fontanelles, dry MM without any visualized tears, no evidence of meningismus, bradycardic without appreciable murmur, Lungs CTA b/l, abdomen soft without organomegaly or distention, no petechiae or bruising, no cyanosis, poor skin turgor with cap refill >2 secs.
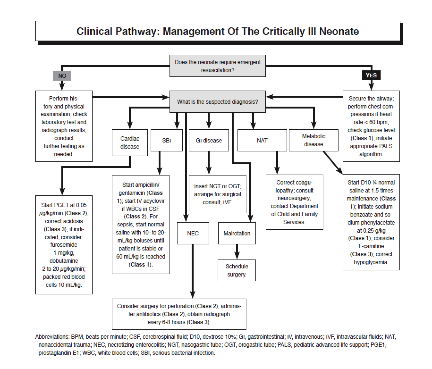
What is your differential and what are your next steps?
DDX: Cardiac disease, Sepsis, GI disease (NEC or malrotation), Abuse, Metabolic Disease, Poor PO intake
Continue below to see what was done. . .
Interventions: IV, O2 (peripheral, central= umbilical, IO), monitor, FS, Labs???
WBC: unremarkable (normal labs for age)
BMP: Na 125, K 6, Bicarb 19, Glucose 40, other labs WNL
UA: neg for infection. Any other tests needed with urine?
UCx and BCx sent, LP not done in ED
What should you do?
- Infants with a suspected IEM should have blood sent for electrolytes, ammonia, liver function tests, and CBC testing.
- The hallmark laboratory finding in IEMs that cause significant deterioration in the neonatal period is an elevated ammonia level. Inappropriate collection (eg, long tourniquet time) or dehydration can cause elevations, but an elevation 3 to 5 times the normal level (ie, above 150-200 μmol/dL) is consistent with an IEM.
- With many of the early presenting IEMs, the definitive diagnosis is made via urine organic acids and/or plasma amino acids, which require 48 to 72 hours for results. Lactate and pyruvate levels may be helpful as well. At some hospitals, these tests are easily sent. At others, ordering may be difficult; in this case, urine and blood can be frozen (in a heparinized plasma tube) for ordering later.
- Patients with salt-wasting forms of CAH typically have hyponatremia, hyperkalemia (in the 6-12 mEq/L range), and low bicarbonate levels. The acidosis is due to hydrogen ion reclamation in the kidney and is not associated with an anion gap unless the dehydration and shock have caused the additional production of lactic acid.
- The lack of steroids renders these patients more susceptible to hypoglycemia, and the glucose level should be checked not only initially, but throughout the course of resuscitation.
- Definitive diagnosis is made with 17-hydroxyprogesterone, dehydroepiandrosterone, androstenedione, and testosterone. These samples must be collected prior to steroid therapy, so extra blood should be held/frozen for use by the endocrinologist before administration of medications.
- If the newborn is hypoglycemic, the glucose level can be corrected more rapidly with use of a D10 5-mL/kg bolus.
- For patients with suspected CAH, hydrocortisone (25 mg) should be given IV or intramuscularly (IM) as quickly as possible, followed by 50 mg/m2/d (roughly 2-3 mg/kg/d) as a continuous drip or divided every 6 hours. Hydrocortisone is the preferred steroid because of its mineralocorticoid effects, but if it is not available, the initial dexamethasone dose is 0.1-0.2 mg/kg IV or IM.
- Patients will require fluid and sodium resuscitation, which can be initiated with 20-mL/kg boluses of normal saline in the ED until stabilization, followed by initiation of maintenance fluids, often initially with dextrose 5% normal saline.
- The hyperkalemia may be impressive, but it is generally well-tolerated. In the absence of ECG changes, it will typically resolve with fluids and hydrocortisone.
- Hyperkalemia associated with ECG changes can be treated in the standard fashion, with care taken not to further dehydrate the patient or cause hypoglycemia. Calcium gluconate (100 mg/kg) is preferred over calcium chloride in neonates.
Mineralocorticoid replacement with fludrocortisone (0.1 mg/d) should be delayed until the patient resumes an oral diet. Disease-specific mortality in the era of screening is 0.7%.
Thanks for reading, leave any comments about the case below!
JK
Jay Khadpe MD
Latest posts by Jay Khadpe MD (see all)
- Morning Report: 7/30/2015 - July 30, 2015
- Morning Report: 7/28/2015 - July 28, 2015
- IN THE STRETCHER INSTEAD OF BESIDE IT - July 22, 2015
- Morning Report: 7/14/2015 - July 14, 2015
- Morning Report: 7/10/2015 - July 10, 2015