Here are the images again.
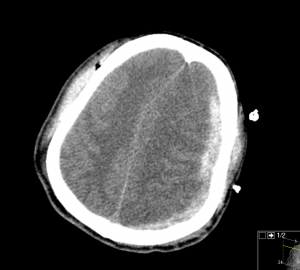
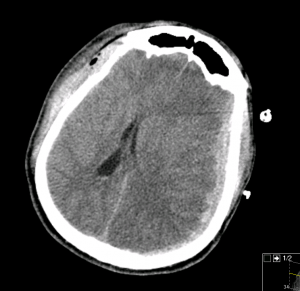
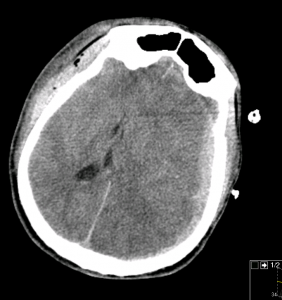
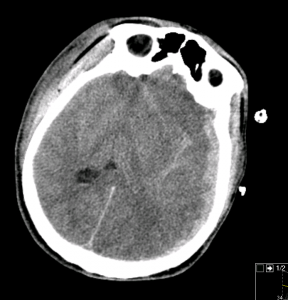
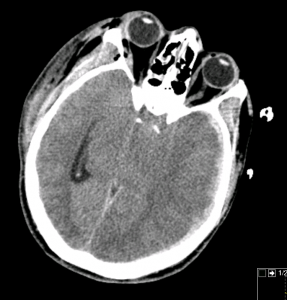
Official read of the CT head: left hemispheric subdural hematoma with significant subfalcine and likely uncal/downward transtentorial herniation.
Traumatic Brain Injury
Impairment of brain function as a result of mechanical force. The clinical severity ranges from very mild to profoundly impaired. The classification of TBI is based on the clinical assessment of a patient’s level of consciousness. The current classification system is based on the Glasgow Coma Scale (GCS).
- Mild – GCS 14-15
- Moderate – GCS 9-13
- Severe – GCS 3-8
Moderate TBI and Severe TBI
Primary Injury: mechanical damage that occurs at the time of head trauma include contusions, hematoma (subdural, epidural, intraparenchymal, intraventricular, and subarachnoid), diffuse axonal injury, tearing and shearing of the tissues, and loss of blood-brain barrier.
Secondary Injury: results from intracellular and extracellular derangement initiated at the tie of trauma by massive depolarization of brain cells and subsequent ionic shifts.
Many cells in the region of damage become necrotic or end in cell death, which activate mechanisms that lead to the production and release of cytokines and other proinflammatory enzymes. During this proinflammatory stage neuronal pathways are interrupted at site and distal to the injury.
In addition, cytotoxic edema (formed within the cell from loss of cell membrane intergrity and ion exchange) and extracellular edema (breakdown of the blood-brain barrier) lead to brain swelling, causing increase ICP. Elevated ICP can cause direct compressive damage to the tissues and lead to ischemia from compression of the vasculature. Results can be herniation and brain death.
Management: the primary goals for patients with moderate or severe TBI are to prevent further secondary brain injury, to identify treatable mass lesion, and to identify other life-threatening injuries. Secondary brain injury is prevented or minimized by correcting or preventing hypoxemia, hypotension, anemia, hyperglycemia, and hyperthermia, and by evacuating intracranial masses.
- History: obtain details of the mechanism (fall: height, motor vehicle collision: speed, type, damage, etc.). Details of the patient’s condition before and after the trauma, medical history, medications, and drug or alcohol intoxication. Ask about symptoms after injury: nausea, vomiting, headache, or visual inpairment
- A/B: hypoxia increase mortality. Patients with severe TBI require immediate airway. Avoid nasotracheal intubation in possible facial trauma or possible basilar skull fracture. Maintain in-line cervical spine stabilization until cervical spine injury is definitely excluded.
- C: In severe TBI a single episode of hypotension doubles mortality. Aggressiver fluid resuscitation may be required to prevent hypotension and secondary brain injury. Guideline recommends systolic blood pressure be maintained > 90 mmHg.
- D: obatin GCS after resuscitation and prior to sedation/intubation. Assess pupil size and reactivity. Decorticate posturing indicate severe injury above midbrain. Decerebrate posturing indicate a more caudal injury.
- Imaging: Consider CT head in patient with GCS <15. According to ACEP consider head CT in patients with a GCS of 15 who are > 65 yo, coafulopathic, or sustained a fall > 3ft or down 5 more stairs.
- ICP: in ED ICP monitor rarely available. Signs and symptoms of increase ICP are headache, nausea, vomiting, seizure, lethargy, hypertension, bradycardia, and agonal respirations. Neurologic deterioration can be measure by comparing sequential GCS scores.
- mannitol: osmotic agent that can reduce ICP within 30mins and effect can lasts up to 6-8hours. Administered in repetitive dose (0.25g/kg-1g/kg)
- hyperventilation: NOT recommended as prophylactic intervention after severe TBI.
Subdural Hematoma
Caused by suddenly acceleration-deceleration or brain parenchyma with tearing of bridging veins. Hematoma forms between the dura mater and arachnoid.
Classified as acute, subacute (within 14days) or chronic (after two weeks). In acute hematomas patients are usually unconscious. The need for surgical repair are great for acute and subacute subdural hematomas.
On CT, acute subdural hematomas are hyperdense, crescent-shape lesions that cross the suture lines.
Take Home Points
CT shows: subdural hematoma with uncal herniation
Management:
- ABCDEF (Airway is CRITICAL)
- Trauma consult and neurosurgery consult.
Beware of hypoxia and hypotension.
Ultimately, a patient like this one needs decompressive craniectomy and evacuation of the subdural hematoma.
By Joyce Wang
References:
Rudzinski J.P., Pittman L.M., Uehara D.T. (2011). Chapter 268. Shoulder and Humerus Injuries. In Tintinalli J.E., Stapczynski J, Ma O, Cline D.M., Cydulka R.K., Meckler G.D., T (Eds), Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 7e.
Marx, John, Robert Hockberger, Ron Walls, James Adams, and Peter Rosen. “Head Trauma.” Rosen’s Emergency Medicine : Concepts and Clinical Practice. 7th ed. 2010. Print.
jwang
Latest posts by jwang (see all)
- Xray Vision Answer - May 24, 2015
- Xray Vision: My Arm Looks Funny…. - May 16, 2015
- Xray Vision: Limping Answer - April 27, 2015
- Xray Vision: Limping - April 17, 2015
- Xray Vision: Answer - March 27, 2015